Kibong’oto: The History of Global Tuberculosis Control seen through Local Archives
Michael 2019; 16: 270–92.
Tuberculosis (TB) and its control have held an important place in global health since the return of the disease came up for discussion in the 1980s. However, this history is as a rule written from the archives of international institutions like the WHO, making it a history of policies rather than of practices. Using local archives facilitates fresh insight. The building of such an archive in northern Tanzania is presented in this paper. Kibong’oto Hospital has existed as a specialized TB hospital since 1926. Its archive offers insight into a history of TB in diagnosis and treatment that is rather different from that of high income countries, and a story seldom told.
Local and Global Histories of Tuberculosis
Tuberculosis arguably holds a special place in the history of international and global health, which is quite different from what the condition stood for in its previous history. In the 19* century, the control of tuberculosis and other so-called common infectious diseases had been one of the roots of modern public health in industrialized societies. Tuberculosis had become understood as a bacterial infection from 1882 through Koch’s discovery of the tubercle bacillus.*Gradmann (2009). However, despite high hopes this discovery did not quickly translate into effective causal therapies. Instead, much of the work directed against tuberculosis was in fact inspired by social medicine. A social epidemiology that, for instance, identified housing and nutrition as the main drivers of an epidemic made it possible to put amends to such causes on the agenda of health politics.*Overviews to be found in Condrau and Worboys (2010); Dubos, Dubos and Rosenkrantz (1987); Smith (1987). Ironically, therapies that are clearly effective by modern standards only arrived when the condition had already been much reduced in industrialized societies.*Overviews in Mercer (2014) ; Wilson (1990). Starting with Streptomycin from 1946, antibiotics and chemotherapies swept away most of the older therapeutic repertoire from gold therapy and Chaulmoogra, through artificial pneumothorax and chest surgery to good food, bed rest and fresh air.*Greenwood (2008). At the same time, the BCG vaccination, which had only seen modest proliferation in the interwar years, became popular in international health campaigns.*Brimnes (2008). As a result, the history of tuberculosis control took a sudden and radical turn. What had been framed as a social disease in high-income countries now became a technology-driven enterprise in international and global health. Vaccines and chemotherapies have become the primary tools in tuberculosis control campaigns directed at its presence in low-income countries.
The history of tuberculosis in international and global health has been studied in some detail. We have syntheses of the larger picture, studies of single national control programmes, such as that of India, and analyses of the historical situation around 1990. It was at this time that tuberculosis seemed to be re-emerging, that multidrug-resistant tuberculosis became recognized as a serious challenge in high-income countries and when national control programmes for it in low-income countries became a blueprint for cost-effective global health interventions.*Amrith (2002); Brimnes (2016); Gradmann (in print); McMillen (2015); Cf. Ryan (1993). Such histories often focus on institutional actors in international health, such as the Medical Research Council, the World Health Organization, the World Bank or the International Union against Tuberculosis and Lung Disease. They were also written using the archives of such organizations. For all their virtues, they tend to be histories of policies rather than of practices. What is missing are accounts that cover local stories, and that can enlighten us about several interesting questions. How relevant were global policy changes with regard to the history of control in regions or countries? Are there local drivers of change that are overlooked when one choses the eagle-eye perspective of big players in international and global health? What other than plainly positive effects can we attribute to standardized therapy with antibiotics and chemotherapies? The latter question is particularly relevant for the time since about 1990, when such approaches became enshrined in a global health control strategy known as DOTS.*See Gaudillière, Gradmann and McDowell (in print); on DOTS: Gradmann (in print); Ogden, Walt and Lush (2003).
Writing other histories can be inspired by several studies of recent tuberculosis control in global health that social scientists have undertaken, e.g., untangling the notion of patient compliance to combination therapy, or studying the effects that practicing DOTS had on physicians and their clinical skills.*Farmer (1997); Harper (2010); Koch (2013) for a start. It also seems a promising approach to improve historiography to consult different archives that help facilitate the asking of questions about local trajectories. This paper is a report on the creation and exploration of such an archive. The archive in question is that of the Kibong’oto Hospital, which is situated in northern Tanzania on the slopes of Mt Kilimanjaro close to the town of Sanya Juu, a region mostly inhabited by the Chagga people.*Moore and Puritt (1977); Myhre (2018). As you can see on the map in Figure 1, it may look somewhat peripheral in Tanzania, but is situated not far from the road from Dar es Salaam to Nairobi, and is well connected to the nearby towns of Arusha and Moshi.

Figure 1: Map of East Africa.
(Source: Google)

Figure 2: Original building of Kibong’oto Hospital. It was demolished in 2018.
(Photo: Christoph Gradmann)
The hospital’s creation considerably preceded Tanzanian independence in 1961, and if we imagine a map of British East Africa with Tanganyika, Kenya and Uganda, the hospital sits right in the middle. It was in fact created as a small sanatorium in 1926 on the premises of a former German coffee plantation.*Gordon (1961); Titmuss (1964); Wilcocks (1935). By that time, the number of beds was between 10 and 20. The institution received more patients in particular from the Second World War. In the 1950s, it became expanded in building mass and function to a tuberculosis hospital that would have approximately 200 beds and handle thousands of patients per year. In those days, it would attract patients from all over British East Africa and even beyond. After independence, business showed no sign of slacking. However, the patient population seems to have become more national in composition – Kibong’oto being after all the country’s only specialized hospital for that condition. In its late colonial days, there is some evidence that quite a bit of research was also done there, mostly trials on domiciliary treatment by C.G. Gordon. Notably, these trials took place roughly in parallel with the well-known MRC trials on the same question in Madras/Chennai, which were begun in the late 1950s.*Gordon (1961); McMillen (2015: 138-40). Since the late 1970s, we find that clinical drug trials were based there. It seems that it was with the creation of the Tanzanian National Tuberculosis and Leprosy Programme from 1977 to 1987 that Kibong’oto lost much of its standing in the country.*Information on the hospital’s history can be collected from some published work: Clyde (1962); Davies (1938) Gradmann (in print). In a centralized system run from Dar es Salaam through district control officers, Kibong’oto had become an anachronism. Ironically, one could say, the hospital was saved by drug resistance. In the early 2000s, Kibong’oto became a national referral hospital for MDR TB, and with political commitment and an energetic director, generally experienced an upswing inspired by MDR treatment and research.*This information was drawn from annual reports that we received from the National Tuberculosis and Leprosy Control Programme (https://ntlp.go.tz/), and from interviews conducted with former employees at the Kibong’oto hospital in Dar es Salaam in June 2017. So in a sense, while it was threatened with oblivion by the creation of the NTLP, in which all functions such as district control officers, drug sensitivity laboratories and the like became located to the nearby town of Moshi, Kibong’oto was saved by MDR TB, currently holding the impressive title of the Kibong’oto Infectious Diseases Hospital (KIDH), being a centre of research, treatment and training in relation to tuberculosis and other respiratory conditions.
Fortunately, we are in position to gain some inside perspective of the hospital’s daily clinical business throughout most of its existence. From 1926 to the early 2000s, employees condensed their daily activities in diagnosis, treatment and research into a library of casebooks. Casebooks, which are summaries of patient information, are a genre of medical text that has existed for centuries, and that has successfully been employed in the histories of medical knowledge and its production.*For an introduction to the genre, see Craig (1990a, b). Sadly, while this library seems to have been kept meticulously over a long period of time, it was disposed of around 2010, presumably when the hospital switched to IT-based documentation systems.*Oral communication from Alexander William Mbuya. Dumped in a basement, it was on the road to becoming a feast for termites when our project came across it in 2015.

Figure 3: Basement premises from where archival material was recovered.
(Photo: Christoph Gradmann)
Building the archive
In the basement of one hospital building, a large amount of mostly historical equipment and documentation was kept. The material was very mixed and partially damaged due to infestation with mould and termites. One thing that caught the attention of the team was that there were a large number of books hidden under a lot of other material (Figures 4 and 5).
In a first step, these books were recovered and subjected to a cursory inspection if their condition allowed for that. To our delight, it turned out that they pretty much covered the entire period from the founding of the hospital in 1926 to the 1990s. Nevertheless, variations in the state of preservation were considerable, with some beyond recovery. Moreover, variations in content were found to be wide: Most volumes were casebooks, which would usually be grouped by region and which contain summaries of patient histories. Usually ordered by date, many of them came with alphabetical indices, making them powerful tools in everyday clinical practice. Others contained staff lists, records of screenings in the local environment and more.

Figure 4: A pile of casebooks in a corner.
(Photo: Christoph Gradmann)

Figure 5: Infestation with mould and destruction by termites. Some books were beyond recovery.
(Photo: Christoph Gradmann)

Figure 6: Recovering and preserving hospital casebooks.
(Photo: Christoph Gradmann)
Faced with a large number of such books, many of which were in bad shape, a decision was made to establish a collection of approximately 100 such books that would provide some material for all the decades from the 1920s to the 1990s. The aim was to facilitate a comprehensive overview of how tuberculosis treatment was practiced throughout the period and what other activities were documented. This was done by selecting from those books available in reasonable shape. One can argue that a higher number could have been kept. Yet, we decided that a small collection was sufficient for the purposes defined, with several practical considerations leading to that decision. Keeping a larger collection would have meant including many in poor condition that were difficult to restore and keep. A collection of limited size can also be kept in way that would not take too much space and is easy to maintain. Most importantly, this could be expected to cause no conflicts with the primary business of the hospital. Lastly, since no material from the hospital basement was disposed of, it would be possible to expand the collection at a later stage if deemed necessary.
Following a pilot in 2015, most of the work in creating the archive was done by Christoph Gradmann in 2017 and 2018. In recovering the material, he collaborated with Alexander William Mbuya, and was also aided by other members of hospital staff. During the selection and cataloguing, several meetings were held with Alexander William Mbuya, during which progress was reviewed and the way forward discussed. The result was a catalogue of 102 volumes, covering histories from 1926 to the mid-1990s. We also proposed a policy of restricted access to the collection.*Final report for NIMR/HQ/R.8a/Vil.IX/2295, “Trajectories of Tuberculosis: Understanding and Treating Tuberculosis at the Kibong’oto Infectious Diseases Hospital (KIDH) 1926-2016”, 2018. This seems important in the case of a collection that contains quite a bit of, albeit historical, patient information. Access to the collection should only be granted on the condition that, as a general rule, no information able to identify individual patients should be published. It may be argued that many of the patients are long dead, but since this is impossible to determine in individual cases, and in many cases their descendants might live in the vicinity, it seems advisable to err on the side of caution and completely anonymize everyone. We therefore suggested that in addition to the requirements by Tanzanian archival and research laws on future access to the collection once it is ready for use, the right to view it should be exclusively granted through the hospital management and in consultation with an expert historian.
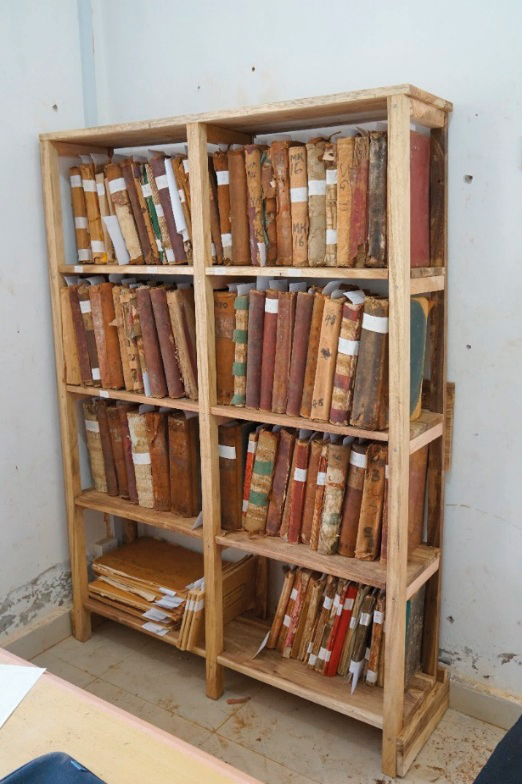
Figure 7: The complete collection as it was kept in 2018.
(Photo: Christoph Gradmann)
The collection was made accessible through a simple database. If still existent and legible, the original signatures were used; if not, new signatures were provided. A catalogue has been written, with copies kept in the hospital and in Oslo. Because the original books were given signatures that reflect the geographical origins of the patients, it is easy to see that the material falls into three broad periods: In the early years until the end of the 1930s, there are only books for local patients (from eastern, middle and western Kilimanjaro). From the 1940s onward, other series appear. First, a series for patients out of Kilimanjaro was abbreviated as SG. In this case, the first surviving book SG IV is from 1942, meaning that the series was probably started not long before that. In the following decades, other series were started covering regions or tribes: Mbeya, Arusha, Pare and Maasai. Later, from the introduction of short-course chemotherapy in 1983, the casebooks were first supplied with- and eventually replaced by comprehensive tabular registers of everyone undergoing such treatments.

Figure 8: The hospital’s autoclave.
(Photo: Christoph Gradmann)

Figure 9: A truck parked on the hospital premises.
(Photo: Christoph Gradmann)

Figure 10: Two stamps, very useful in the everyday clinical application of chemotherapy.
(Photo: Christoph Gradmann)
Beyond the casebooks, there are some material traces of Kibong’oto’s history. The building where it was started (Figure 2) was demolished in late 2018. What still exist are additional newer buildings on the premises. One of them bears a plaquette to commemorate the opening of a spacious building in 1952. The hospital’s laundry still contains a dated but fully functional autoclave. After consultation with experts on the matter, we presume that it is a 1950s model made to look more modern by being painted light blue. When we started our work, there was also a Bedford truck, which – judging from its number plates that start with GT (for Government of Tanganyika) – might well have been the one used in the so-called X-ray safaris that accompanied Dr Gordon’s domiciliary treatment research in the 1950s. Finally, there is a graveyard for patients who were not picked up by their families after their death. It is located in a nearby grove, and was only discontinued around 2010.*Interviews related to and inspection of the graveyard by Christoph Gradmann, 27/28.2. 2018. The only material remains from the clinical practice that could be recovered are two small stamps employed in the diagnosis of tuberculosis. One shows an abstraction of a lung, while the other is suited to enter diagnostic values into textbooks, such as acid-fast bacteria found, tuberculin test, erythrocyte sedimentation rate, haemoglobin percentage and weight. They show signs of heavy use, which is discussed in the next chapter. From what we know, they were continuously used from the 1950s to the 1990s. They seem to have been held in some esteem by the staff. Significantly, they were not found in the basement, but instead in the hospital’s registry. They are now kept with the collection.
Kibong’oto Hospital – selected documents from its archive
The following pages offer a selection of documents from that collection, they are not a history of tuberculosis treatment at Kibong’oto. Yet, the pictures show many dimensions of hospital life and work, including changing diagnostics and therapies, patient careers, which resources were present and which were missing, social relations between patients and health personnel and so forth. Despite the fact that many of the patients whose stories we encounter in the following documents have been dead for quite a long time, we have decided to anonymize all of them by blurring their and their relatives’ names in the illustrations.
Document 1: From WK1 1930, Beginnings
Our first example shows the summing up of a patient history beginning in 1930. It is from casebook WK1, meaning the first such book kept for West Kilimanjaro. In those days, diagnosis relied heavily on interpreting clinical symptoms, in this case fever. Interestingly enough, in our case there is no sharp distinction made between tuberculosis and other respiratory conditions. The patient from the village of Machame, who is introduced as a “Pulmonary Tuberculosis Positive Case” at the outset is said to have “Tuberculous Pneumonia” later on. A diagnosis was done by taking the patient’s sputum to the hospital for microscopic inspection before admission. Treatment in those days would vary from artificial pneumothorax to calcium injection, cod liver oil, chaulmoogra, tuberculin and more. In our case, not much treatment has been attempted, though quinine application is noted. However, this medicine was a treatment for malaria rather than tuberculosis. By contrast, notes on weight and temperature change are meticulous. Also, a husband and two children are tested with tuberculin.
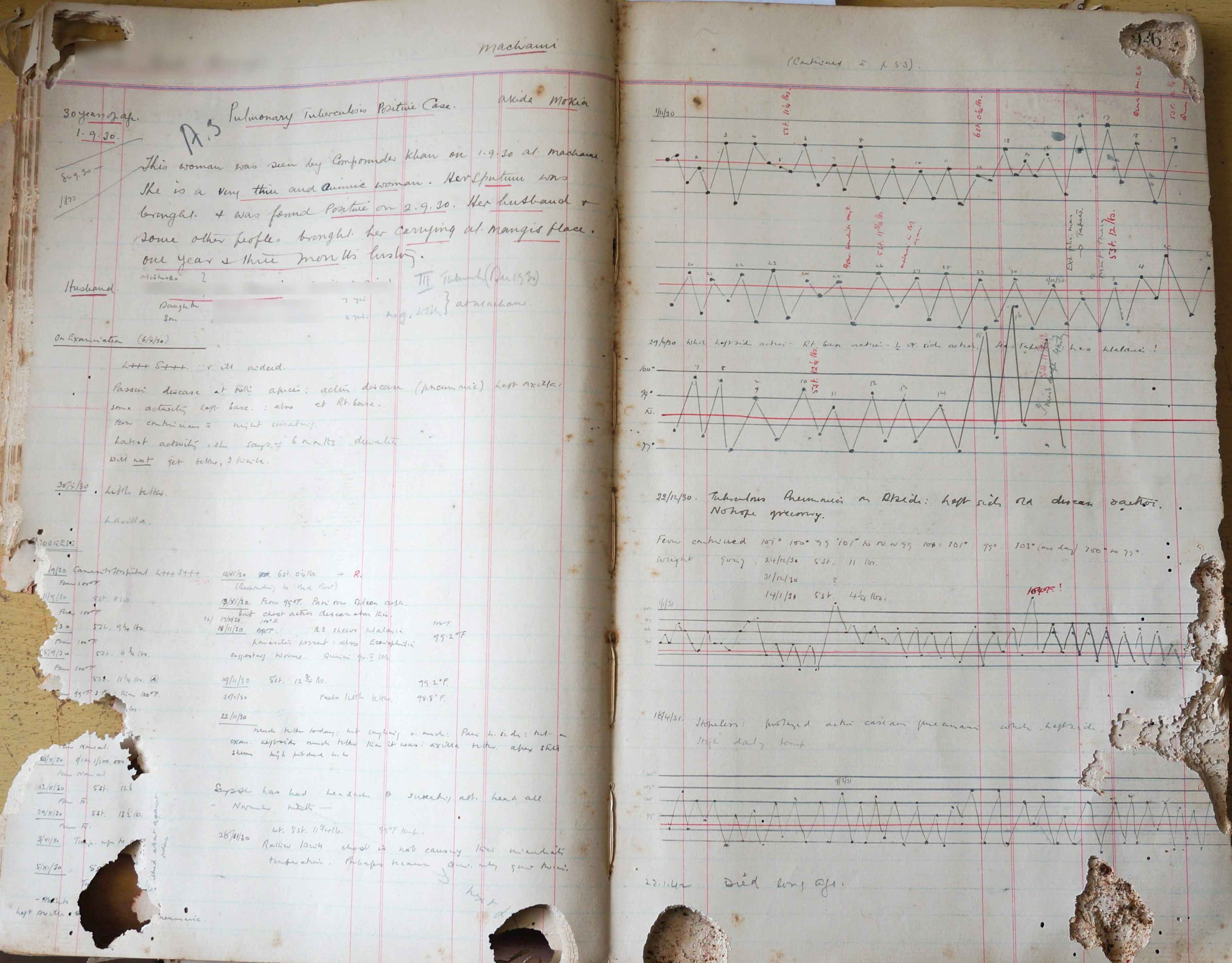
Figure 9.
(Photo: Christoph Gradmann)
A long hospitalization and the testing of relatives with tuberculin were frequent in those days, and our patient seems to have been hospitalized for at least eight months. Not all information is as precise as the use of the fever curve would make us believe. After eight months, further proceeding is not reported. More than a decade later, in 1942, someone added the comment “died long ago”.
Document 2, from SG IV, 1941, Induction Therapy
SG books document patients from outside the Kilimanjaro region. This patient came from from Zanzibar.
This document is an excerpt from a longer patient history, covering six pages, and it shows the way the dominant therapy of those days was practiced. Induction therapy was done by injecting air between the pleura and the lung. The idea was to inhibit the circulation of air in parts of the lung, and thereby put to rest and isolate those parts affected by tuberculosis. This had become possible at Kibong’oto some time during the 1930s. Generally speaking, induction therapy was the most popular treatment of tuberculosis in the first half of the 20* century.
There are three columns on the page we see showing the dates of the injection, where the injection was placed in the lung and finally how much air was used. As we can see, injections had to be renewed frequently, making the therapy labourious and time-consuming. In July 1941, the treatment is given up, with a microscopic investigation of the patient’s sputum revealing many bacilli. The value ++++ indicates the highest possible count, the patient is reported to be “coughing much” and released with the comment, “May well die on the way”. Death is reported, presumably from outside the hospital, in August 1941.
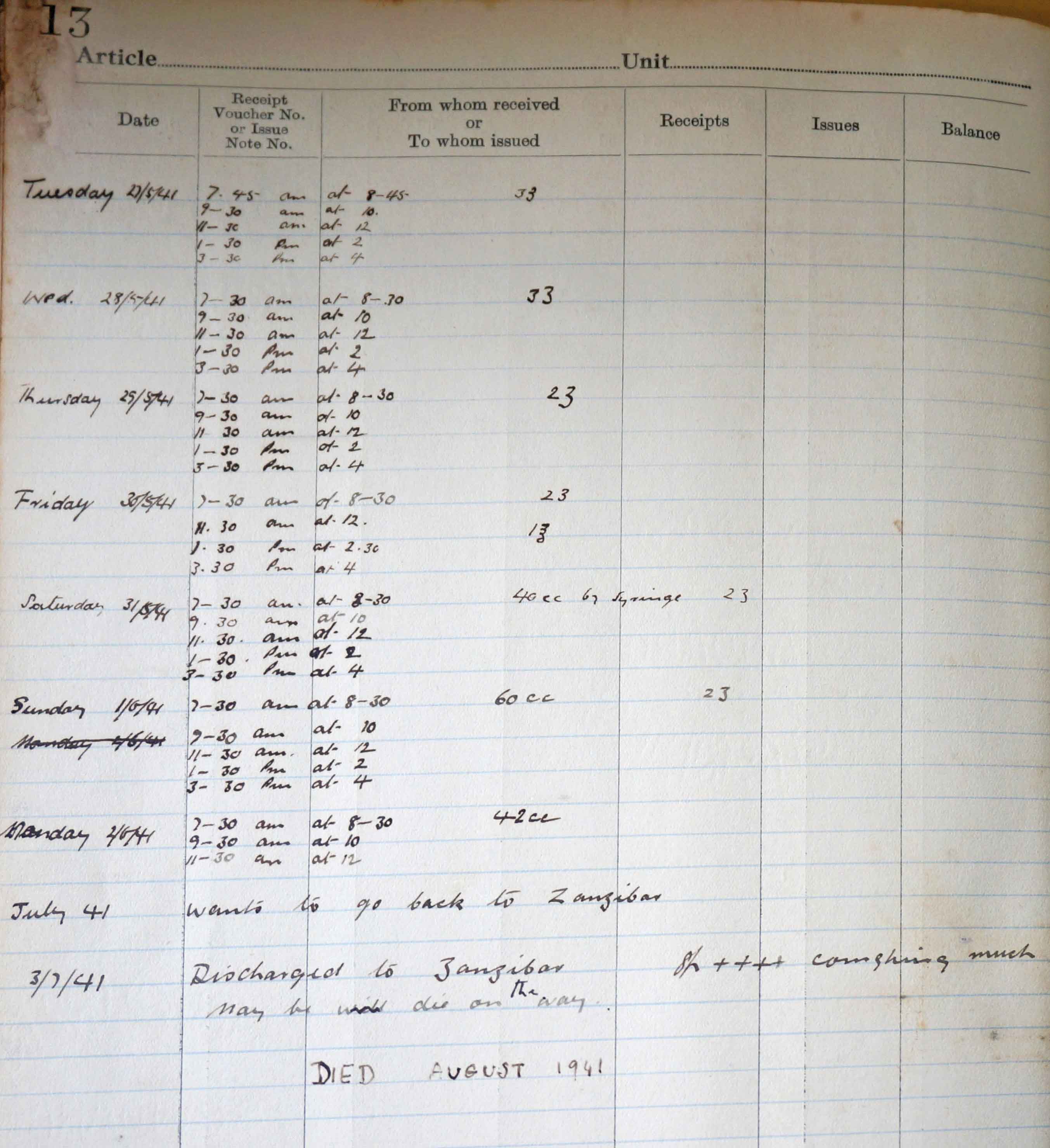
Figure 10.
(Photo: Christoph Gradmann)
Document 3, MK 16, 1957, Chemotherapy Arrives
This patient is from Middle Kilimanjaro (MK). What we see is the unexpectedly happy ending of a much longer history, and it involves switching from induction therapy to treatment with antibiotics and chemotherapy. Initially, the patient is readmitted and reported to have “missed his refills for three months”. We understand the patient had been non-compliant to induction therapy, the refills being refills with air. Modern chemotherapeutic treatment arrives as the solution to the patient’s treatment and lack of compliance. The patient is hospitalized and receives a combination of streptomycin and PAS for two months, after which he is released for home treatment with isoniazid and PAS. The use of a stamp with a small lung indicates that tuberculosis is now almost exclusively understood as an affliction of the lungs. The use of chemotherapy results in a shortening and standardization of therapy. The other two stamps, used shortly before release, give a list of indicator values to be noted: sputum [bacilli in sputum, in this case none], tuberculin reaction [Positive] and so on. An increase in weight and an absence of bacilli in the sputum indicate progress. Ultimately, the improved patient asks for release, which is granted: “Wants to go to Mombasa for his work as a tailor
----
Yes”.
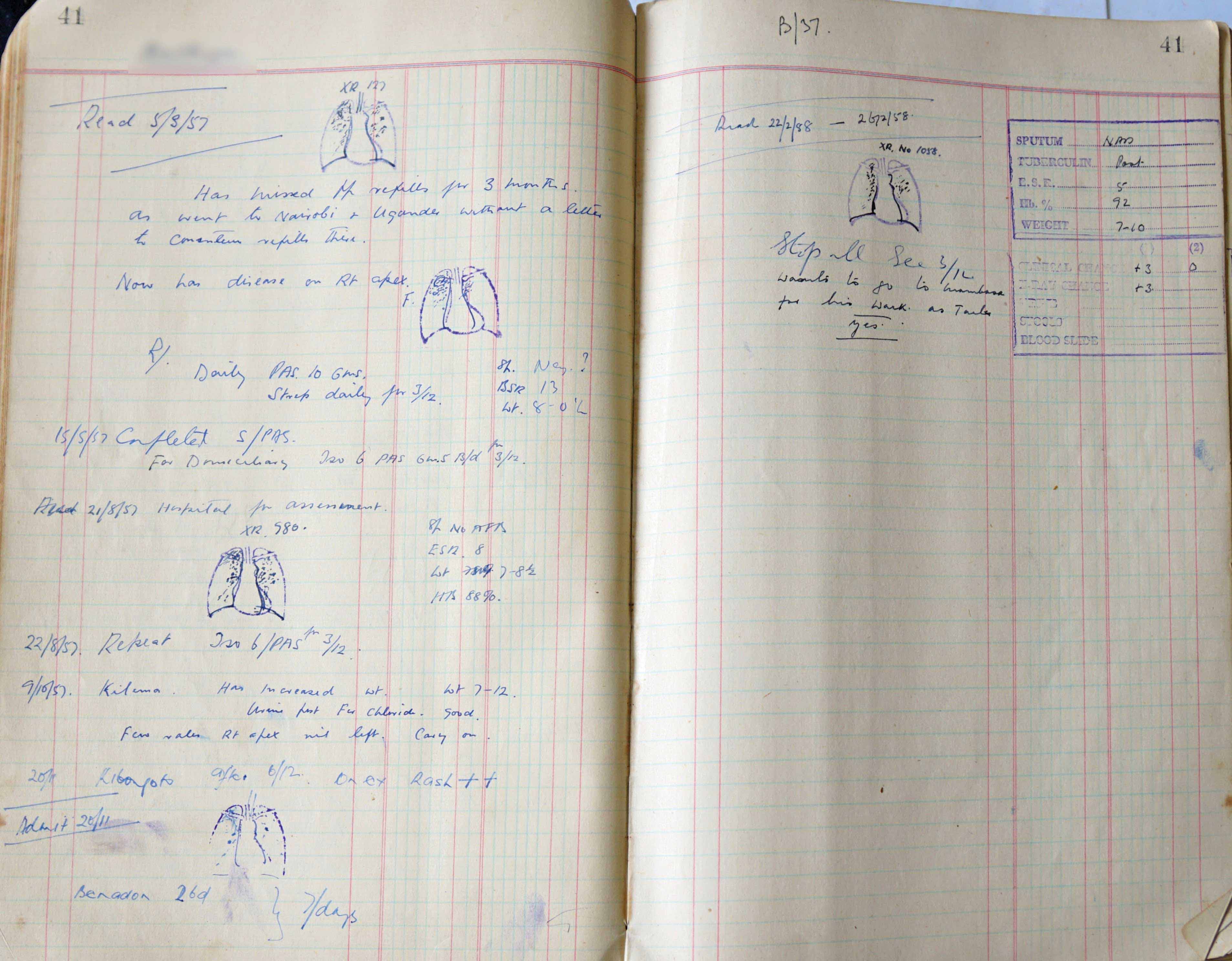
Figure 11.
(Photo: Christoph Gradmann)
Document 4, MB 3, 1957, Tuberculin Screening
Our fourth document (above) shows an activity, which Dr Gordon, the resident specialist in the 1950s, was quite fond of: tuberculin surveys. This one was done in a school in Arusha Town in 1957. Tests are noted with a running number, full names (blurred), the tested individual’s age, and the strength of the reaction, which in this case was noted twice, presumably with some time in-between. In addition, the tribe to which an individual belonged is noted and for those not from Arusha, names of villages are added, like “Chagga [from] Rombo”.
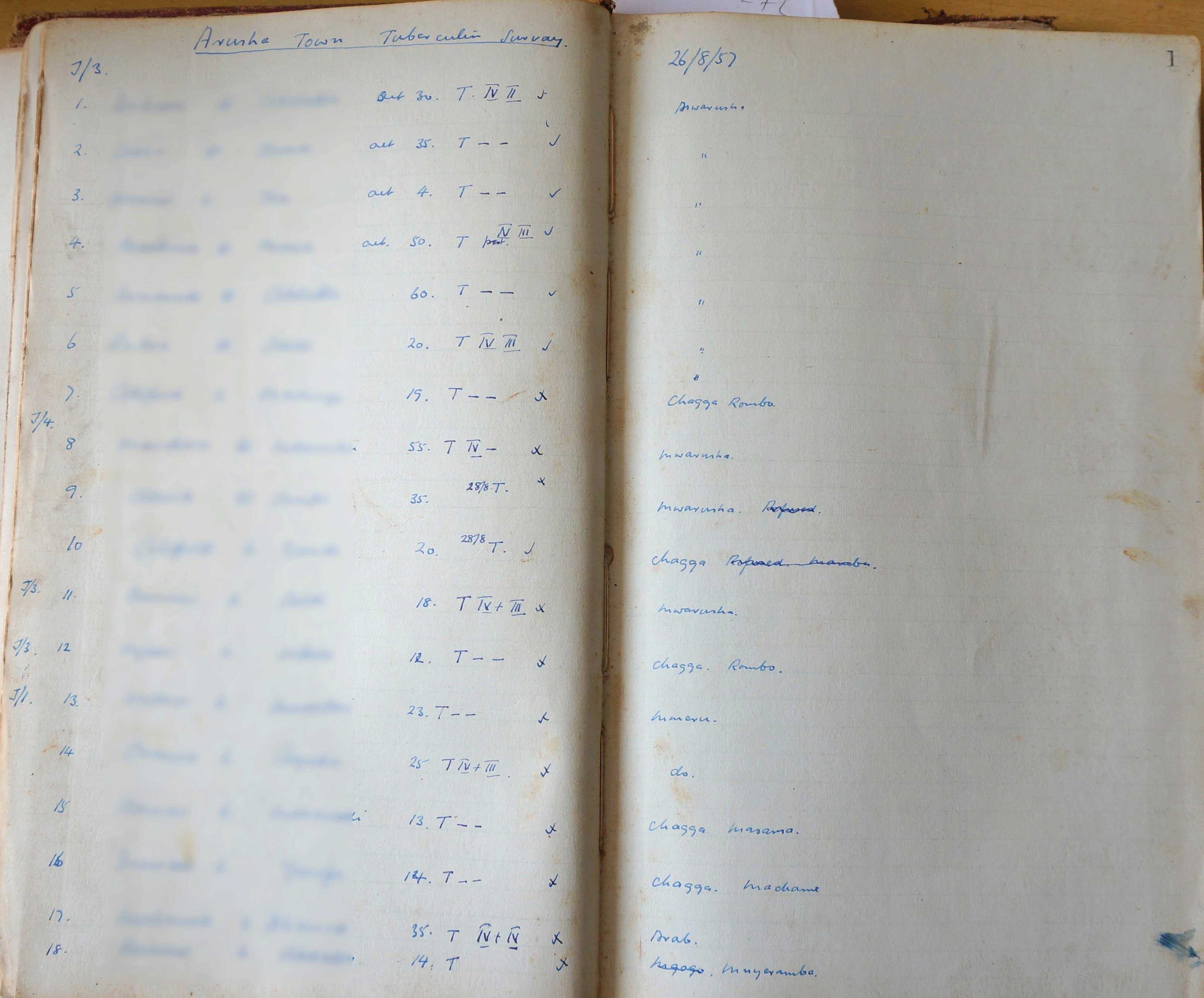
Figure 12.
(Photo: Christoph Gradmann)
Document 5, SG 72 [1976], Elaborate Treatment
We are writing the year 1976, and those were days when Kibong’oto Hospital was able to offer elaborate therapies. In this case, the prestige which the hospital enjoyed is visible through the patient: A patient transferred by a private doctor from Dar es Salaam – in times when private practice was illegal in Tanzania! Noting the information on a patient’s tribe was done on a mandatory basis in those days. Our patient gets the entry, “Tribe Asian”, to which “Relg. Hindu” is added. In addition to his diagnosis with serious pulmonary tuberculosis (PTB+), the patient is said to suffer from asthma. It is not just the referral by a “Private Dr., who has given the patient isoniazid, which indicates a wealthy patient. The patient gets a rather personalized treatment with Rifadin, Myambutol, isoniazid and “extra milk”.
Three things are remarkable here: The diagnosis of PTB+ (for pulmonary tuberculosis plus) despite the absence of bacilli in the sputum. This, we might suspect, owes to previous therapy, though a negative tuberculin reaction, which is also noted, cannot be explained in that way. Remarkable is also the use of the expensive retreatment drug Rifadin – at the time still patented – in the absence of a drug sensitivity test and the use of food as medicine. The latter was widespread in the hospital in the 1970s. In other examples, a patient could get a protein-rich diet as part of their treatment. The status of food as treatment was suspended with the introduction of short-course chemotherapy from 1983. The patient is transferred back to Dar es Salaam after four months of treatment.
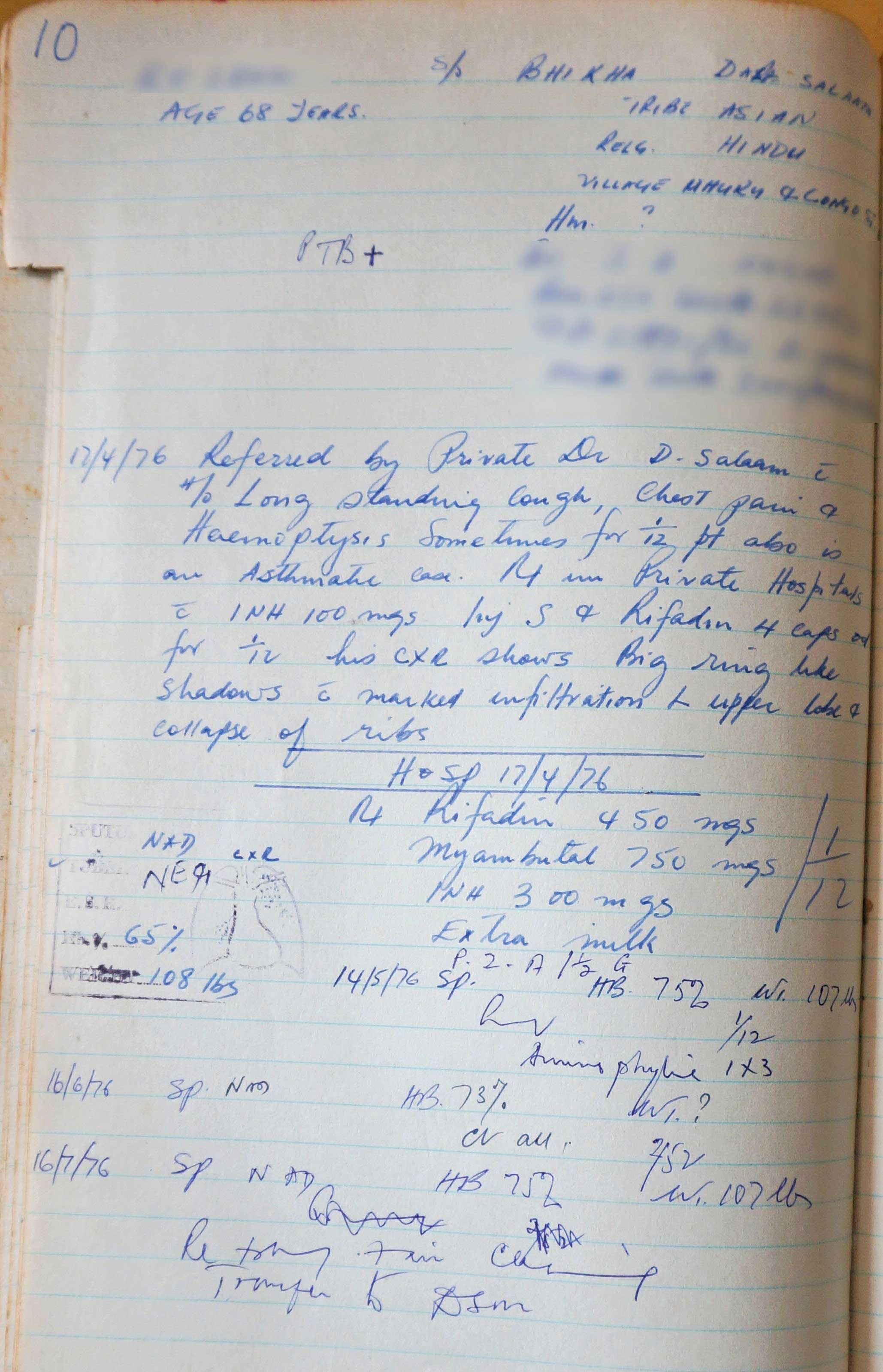
Figure 13.
(Photo: Christoph Gradmann)
Document 6, MS 14 [1976], Multi-drug Resistance
This is a patient from 1976. It is from a dedicated series of casebooks for Masaai patients, presumably started in the 1960s. The patient has a prehistory of treatment at St. Francis Hospital in Ifakara, employing most of the available medicines from those days. Clearly, a transfer to Kibong’oto is seen as a way out and last resort for both St. Francis and the patient. The patient, who is 65 years old, turns out to be one of the first MDR patients to be documented in the files. The sensitivity test result seems to arrive about five months after admission, and it shows a resistance to isoniazid and streptomycin “Sensitivity Test ISO R STREPT R”. The patient then goes on what was an expensive retreatment regimen in those days. The patient is ultimately “awaiting discharge” with drugs for one month, perhaps to be returned to Ifakara.
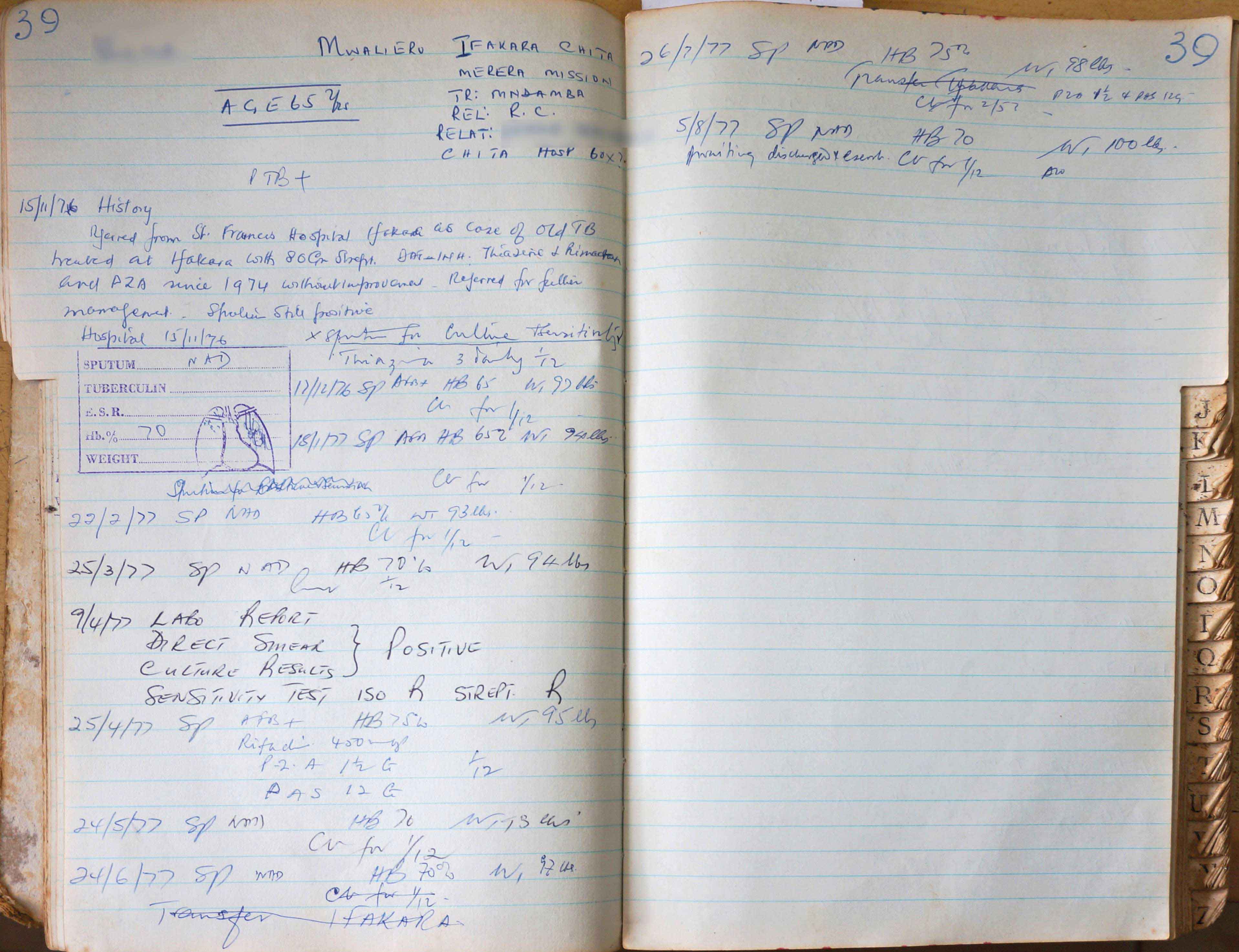
Figure 14.
(Photo: Christoph Gradmann)
Document 7, MS 14 [1986], Absconding Patients and Teamwork
What is remarkable in the story that this file tells is less the treatment than what we can learn about the social world of the hospital. As has been the rule throughout most of Kibong’oto’s history, the patient’s story is reported in many different handwritings. This was also the case in document no. 5, and it is the rule in any case written down after the Second World War. What we could naively assume to be the work of the resident specialist (there was usually only one) is actually the work of a much larger number of medical officers, laboratory workers and nurses. We know that they were numerous, and did the bulk of all work with the patients at least since the 1940s. To give one example, in 1968 the hospital had one specialist physician, one medical assistant, one microscopist, one laboratory assistant and 56 nurses.
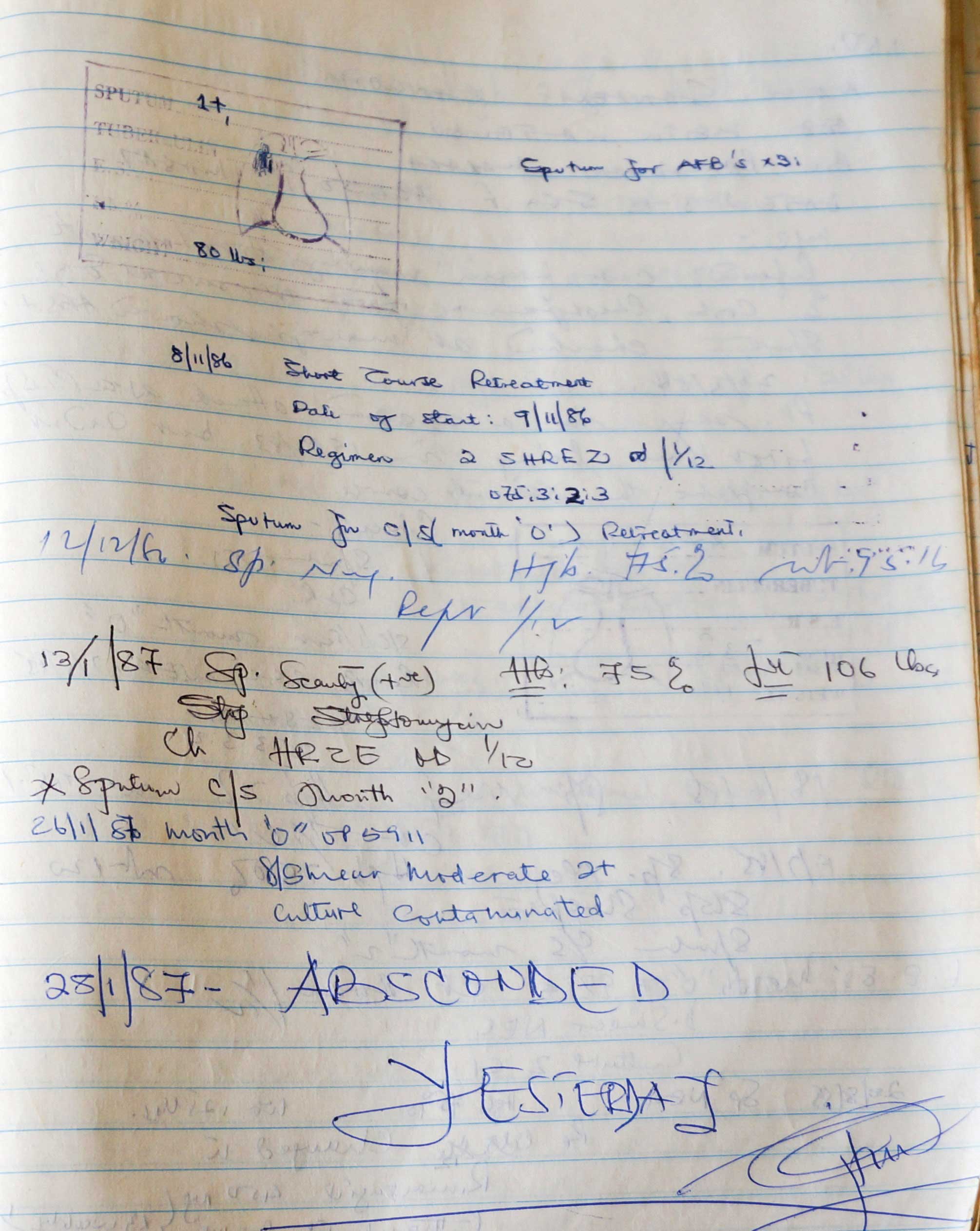
Figure 15.
(Photo: Christoph Gradmann)
The other remarkable thing is the fact that the patient ran away. This was by far the most common type of conflict in the hospital reported in the casebooks. Not infrequently, such patients were returned later on by their families. This was not the case here, where someone noted in unusually big and capital letters “ABSCONDED YESTERDAY”. We can almost sense the author’s frustration and anger!
Another very common social activity, which is in some sense complementary to absconding, is self-referral, with patients coming to the hospital and asking for treatment. This is quite frequent.
Document 8, 1983/1 August 1983, Making DOTS
This document from July 1983 indicates the start of short-course chemotherapy in Kibong’oto Hospital. Since August 1982, the International Union against Tuberculosis and Lung Disease had been implementing it in Tanzania’s national tuberculosis control programme, advancing district by district. Once completed, this programme became the blueprint for the WHO’s DOTS strategy in the 1990s.
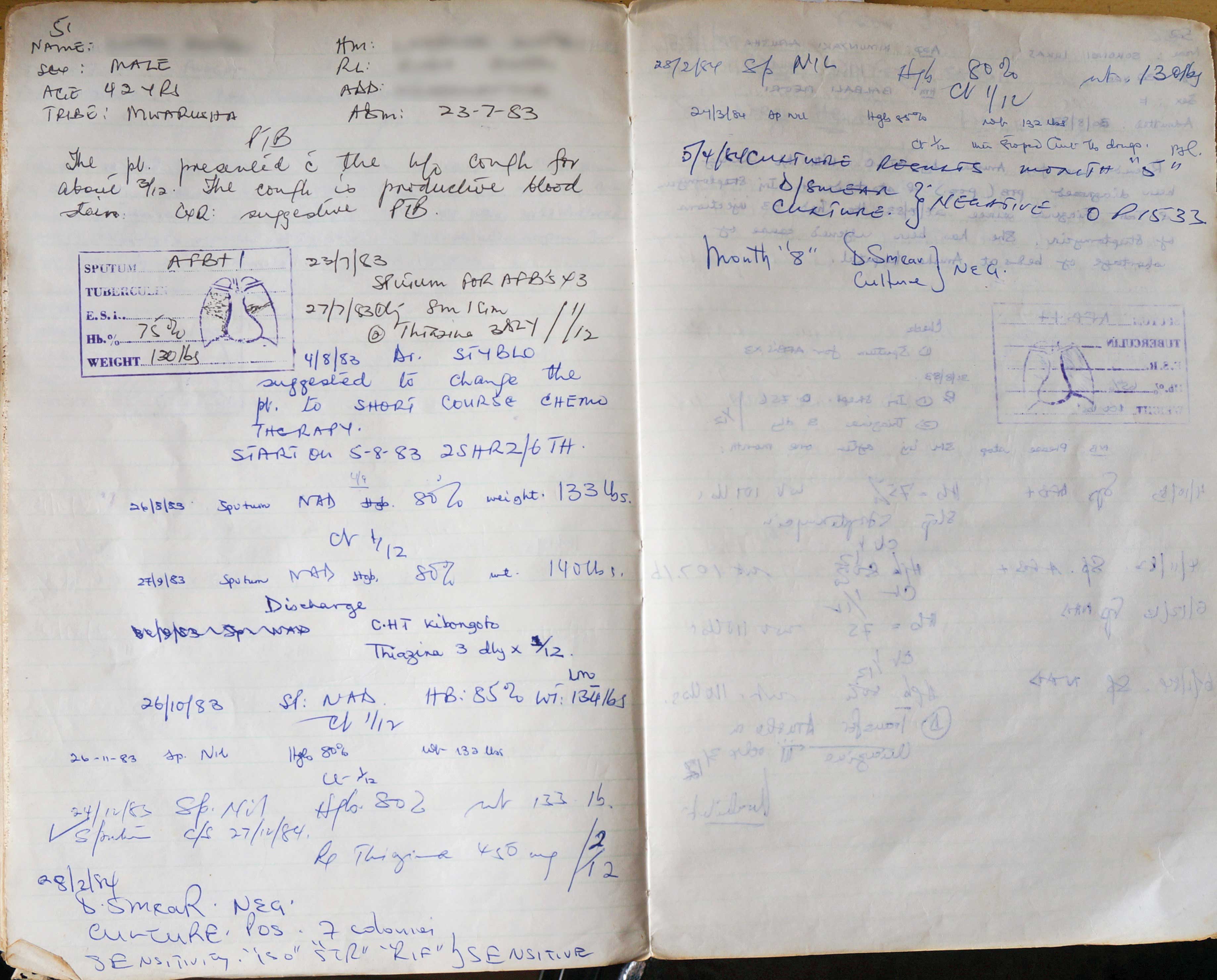
Figure 16.
(Photo: Christoph Gradmann)
In Kibong’oto, the IUATLD consultant in charge, Karel Styblo, came as a visitor. For 4.8.1983, it is noted: “Dr. Styblo suggested to change the pt. to Short-Course Chemotherapy. Start 5.8.83.” Treatment starts with two month on streptomycin, isoniazid, rifampicin and pyrazinamide, and continues with six month of Thiazina and a fixed-dose combination of isoniazid and thioacetazone. Note at the bottom of the page that the patient is given a sensitivity test. This is very unusual in the case of patient with no pre-treatment history or complications, and illustrates the air of novelty and innovation that surrounded the introduction of short-course chemotherapy. The release date for home treatment was two-and-a-half months after admission, and on the subsequent page we learn that the patient, whose sputum had been bacilli-free upon release, is declared cured after eight months. For all we know, this was a standard procedure in the Tanzanian programme, and it became a DOTS standard later on.
Document 9, Short-Course Chemotherapy [1983]
This is a page from an entirely new type of documentation that only appears together with the introduction of short-course chemotherapy at Kibong’oto Hospital from 1983. The more textual documentation that we have seen in the earlier casebooks became supplemented by tabular overviews of the below type. The traditional case summaries continue to be written in parallel, but are abandoned after about a decade, in the mid-1990s. The tabular overview allows for little but writing down the standardized readings of laboratory values, whether or not there are bacilli to be found at months 5 or 8 of the treatment regimen, as well as references to other files. The numbers below “Reference” refer to the standard DOTS regimen, in which the continuous application of drugs would be accompanied by controls at months 0, 2, 5, 8. They testify to a substantial increase in the standardization of diagnosis and therapy, which arrived part and parcel with short-course chemotherapy. There were, and not just on this page, substantial numbers of defaulters. This seems to shed some doubt over the 90% rate of successful treatments that the NTLP was credited with in IUATLD reported in those days.
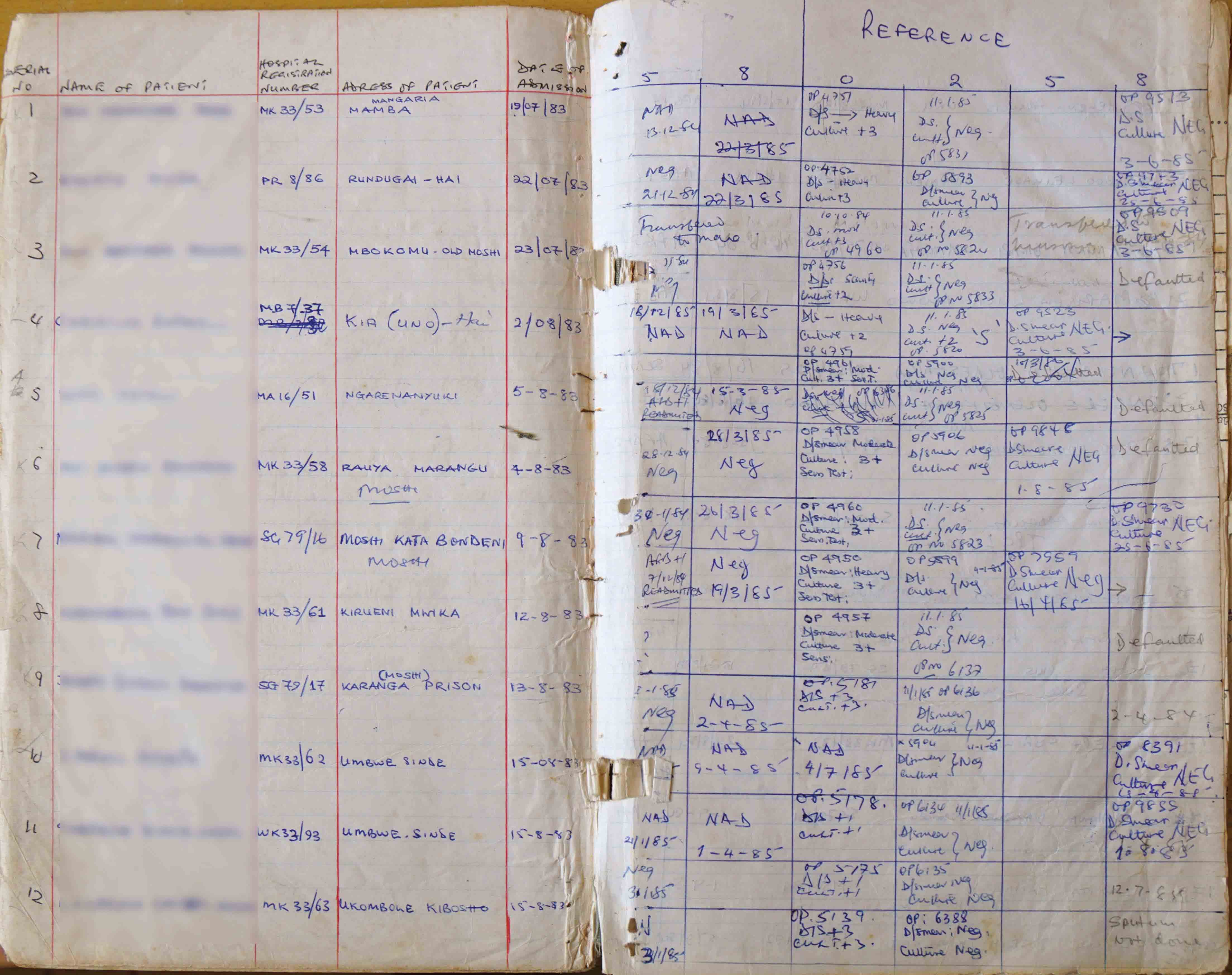
Figure 17.
(Photo: Christoph Gradmann)
Document 10 a b c, [1991/1], AIDS
In the casebooks, HIV or AIDS, as it would then be called, appeared from 1985. The patient from a casebook from 1991 is reported to be in extremely bad shape and arrives with an HIV diagnosis after having been transferred from Karagwe Hospital through KCMC. Contrary to the very standardized treatment of pulmonary tuberculosis patients, the diagnosis and treatment are rather explorative. While diagnosis is under way, to “encourage feeding” is specifically noted for this very wasted patient.
Once therapy commences, the patient starts on a normal DOTS regimen (SHRZ), but is immediately given INH and Ethambutol as a continuation instead of Thiazina, as would have been commonly done previously. HIV patients were in danger of violent skin reactions to thioacetazone (Stevens-Johnson syndrome), one of the component medicines in Thiazina. The snippets above from 1991 and 1992 show two such reactions, which invariably resulted in dropping Thiazina and switching to a combination of INH and Ethambutol.
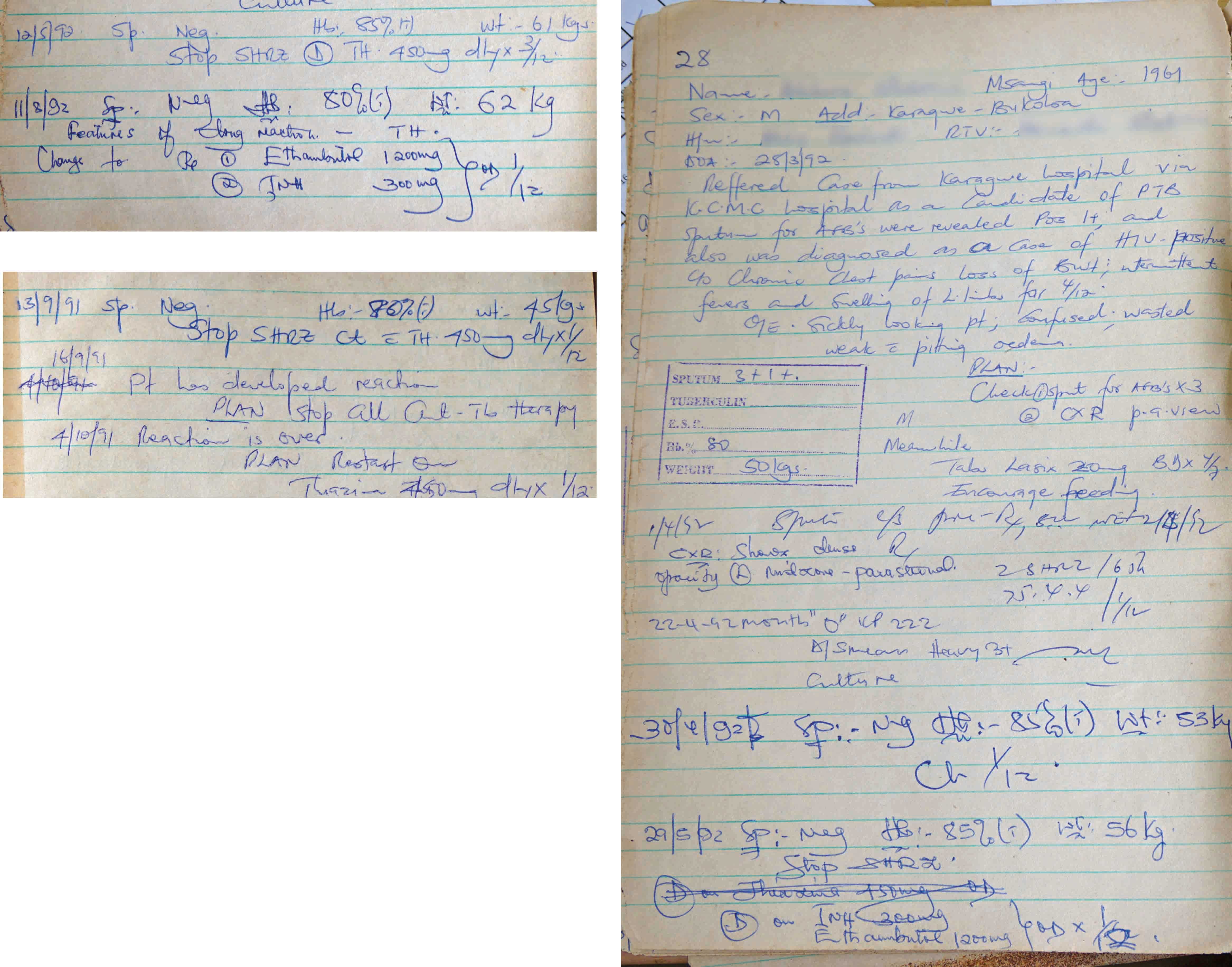
Figure 18 a-c.
(Photo: Christoph Gradmann)
Document 11, MK 33, 1983, Sensitive Issues
The story of this patient from 1983 is sad, but by no means uncommon. A sensitivity test is ordered, but the patient is no longer alive when the results arrives. In this case, the results arrives after four months, which by contemporary standards could be considered fast. Delays between six and nine months were not the exception. In fact, it looks like getting such a diagnosis took quite a bit longer after the introduction of SCC than before. Building up the NTLP had increased the demand for sensitivity testing in Tanzania, but plans to expand the available laboratory capacity failed. Things did not always end as dramatically as in this case, in which the patient was dead when the results finally came. However, as becomes clear from other documents, the status of such tests changes from information to confirmation. Second-line therapy would usually be started long before the results of a sensitivity test were available.
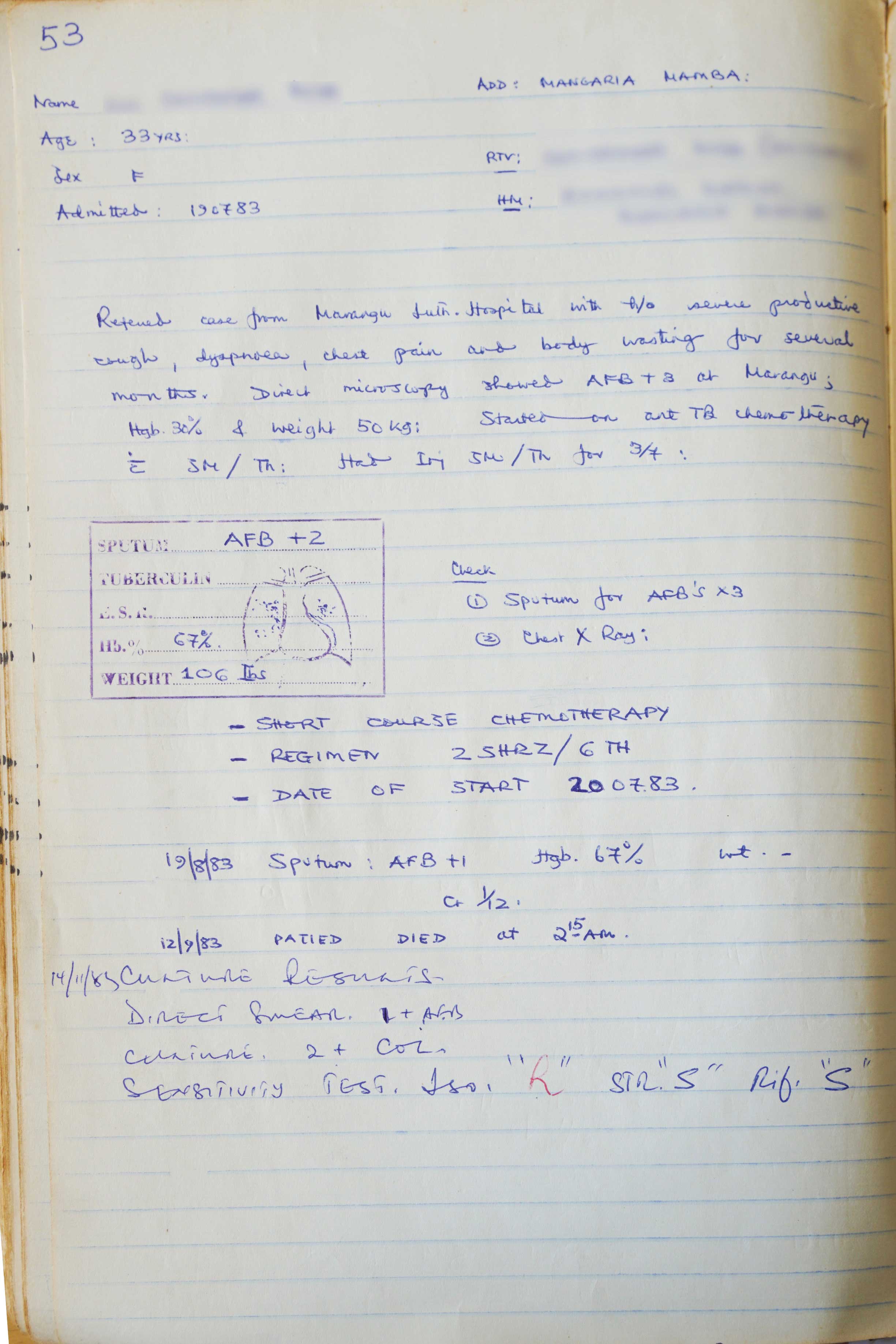
Figure 19.
(Photo: Christoph Gradmann)
Document 12, Clinical Trials, SG 72, 1976
Ultimately, a partial destruction of the archive was carried out by termites from about 2010. However, the disintegration started much earlier, and in this entry from August 1976 we see one of the ways in which it occurred: From the late 1970s Kibong’oto Hospital participated in several clinical trials. What presumably alleviated the hospital’s poor economic condition had problematic effects for the casebook library. Until then it had been comprehensive, telling stories about any patient the hospital’s personnel dealt with. In that way, it had been possible to follow patients’ histories over many years, to spot returning patients, to look at their families and so forth. However, by entering a clinical trial, this remembrance is interrupted. Entries such as “Study x” invariably result in the treatment story being omitted from the casebooks. No values are entered into the stamps, and no documentation of a diagnosis or treatment done in the hospital follows. Rather than being accessible to anyone consulting the books, the information is now owned by those controlling the trial. However, to the best of our knowledge, casebooks on trials were not part of the casebook library.
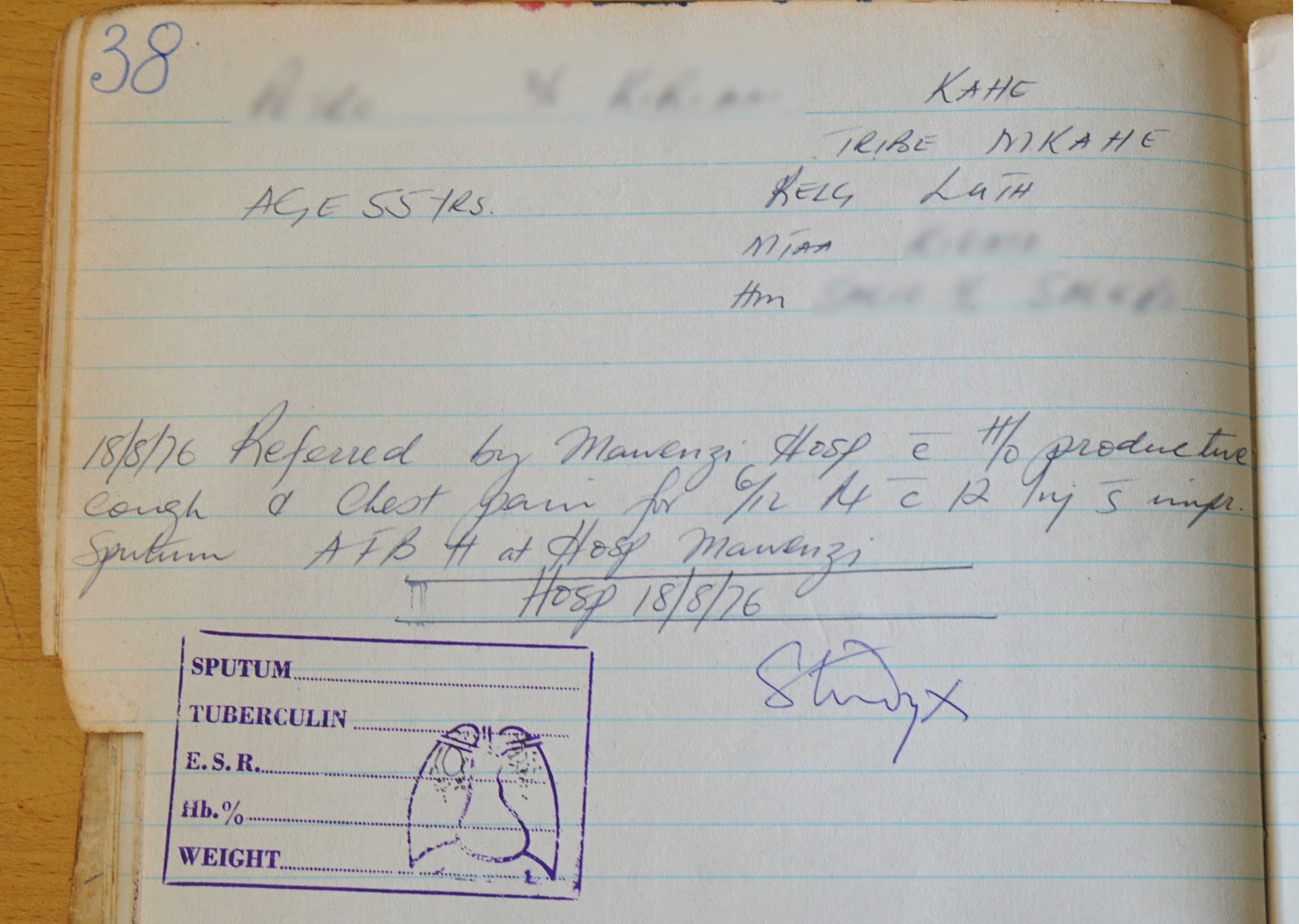
Figure 20.
(Photo: Christoph Gradmann)
References
Amrith, Sunil. 2002. “Plague of poverty? The World Health Organization, tuberculosis and international development, c. 1945–1980.” PHD thesis University of Cambridge.
Brimnes, Niels. 2008. “BCG vaccination and WHO’s global strategy for tuberculosis control 1948–1983.” Social Science & Medicine 67 (5):863-873.
Brimnes, Niels. 2016. Languished Hopes: Tuberculosis, The State and International Health in Twentieth Century India. New Delhi: Orient Black Swan.
Clyde, David F. 1962. History of the medical services of Tanganyika.
Condrau, Flurin, and Michael Worboys, eds. 2010. Tuberculosis then and now: Perspectives on the History of an Infectious Disease. Montreal: McGill-Queens University Press.
Craig, Barbara L. 1990a. “Hospital records and record-keeping c.1850-c.1950. Part 1: The development of records in hospitals.” Archivaria (29):57-87.
Craig, Barbara L. 1990b. “Hospital records and record-keeping c.1850-c.1950. Part II: The development of record-keeping in hospitals.” Archivaria (30):21-38.
Davies, H. N. 1938. “The Work of a Tuberculosis Unit in East Africa.” Tubercle 20 (2): 76-88.
Dubos, René Jules and Jean Dubos, eds. 1987. The white plague: Tuberculosis, man, and society. New Brunswick: Rutgers University Press.
Farmer, Paul. 1997. “Social scientists and the new tuberculosis.” Social Science & Medicine 44 (3):347-358..
Gaudillière, Jean-Paul, Christoph Gradmann, and Andrew McDowell. In print. “The not so distant past, tuberculosis and the DOTS challenge.” In From International to Global: Knowledge, Dieseases and the Government of Health, edited by Claire Beaudevin, Jean-Paul Gaudillière, Christoph Gradmann, Anne Lovel and Laurent Pordie. Manchester: Manchester University Press.
Gordon, C. G. 1961. “A Method of Controlled Home Treatment of Pulmonary Tuberculosis in Tanganyika.” Tubercle 42:148-158.
Gradmann, Christoph. 2009. Laboratory Disease: Robert Koch’s Medical Bacteriology. Baltimore: Johns Hopkins University Press.
Gradmann, Christoph. in print. “Treatment on Trial: Tanzania’s National Tuberculosis Program, the International Union against Tuberculosis and Lung Disease, and the Road to DOTS, 1977-1991.” Journal of the History of Medicine and Allied Sciences: 27 p.
Greenwood, David. 2008. Antimicrobial Drugs. Chronicle of a Twentieth Century Triumph. Oxford: Oxford University Press.
Harper, Ian. 2010. “Extreme condition, extreme measures? Compliance, drug resistance, and the control of tuberculosis.” Anthropology & Medicine 17 (2):201-214.
Koch, Erin. 2013. “Free Market Tuberculosis: Managing Epidemics in Post-Soviet Georgia.” In. Nashville, TN, USA: Vanderbilt University Press.
McMillen, Christian W. 2015. Discovering Tuberculosis: A Global History, 1900 to Present. New Haven: Yale University Press.
Mercer, Alexander. 2014. Infections, Chronic Disease, and the Epidemiological Transition. Rochester: University of Rochester Press.
Moore, Sally Falk, and Paul Puritt. 1977. The Chagga and Meru of Tanzania. Vol. 18, Ethnographic survey of Africa. London: International African Institute.
Myhre, Knut Christian. 2018. Returning life: Language, life-force and history in Kilimanjaro. Vol. 32, Methodology and History in Anthropology. New York: Berghahn Books.
Ogden, J., G. Walt, and L. Lush. 2003. “The politics of ‘branding’ in policy transfer: The case of DOTS for tuberculosis control.” Social Science & Medicine 57 (1):179-188.
Ryan, Frank. 1993. The forgotten plague: How the battle against tuberculosis was won - and lost. Boston: Little, Brown.
Smith, Francis Barrymore. 1987. The retreat of tuberculosis 1850-1950. London: Croom Helm.
Titmuss, Richard M. 1964. The Health services of Tanganyika: A report to the government. London: Pitman.
Wilcocks, Charles. 1935. “Tuberculosis in the natives of Tanganyika territory.” Tubercle 16:31-47.
Wilson, Leonard G. 1990. “The Historical Decline of Tuberculosis in Europe and America: Its Causes and Significance.” Journal of the History of Medicine and Allied Sciences 45:366-396.
University of Oslo, Institute for Health and Society, Oslo / Norway
Centre de Recherche Médicine, Science, Santé, Santé Mentale, Société,
Villejuif/France
Department of Community Health, Kibong’oto Infectious Diseases Hospital, Sanya Juu, Tanzania
