The beginning of the NHS – and the impact on Norwegian health care
Michael Quarterly 2011;8:476–89.
The reason for us in Norway to keep an eye on what happens to the British National Health Service is related to the mutual influence of ideas and social policies between our countries, which has been particularly reinforced during and after the Second World War. The Norwegian government, as well as the King, several influential public servants and labour union leaders all took refuge in London during the war years. The ideas launched by the Beveridge Commission in 1942 set the pace for major reforms in post-war Britain, and inspired Norwegian welfare programmes as well, with gradual reforms leading to free – or almost free – access to health care and education for all.
While Britain started its National Health Service, with its motto «free for all at the point of use», in a major 1948 reform, Norwegian health care has moved more gradually towards the same goals, although since 1969 Norway has also had comprehensive publicly financed health care. As in Britain, general practitioners have a more independent status than hospitals. However, British general practice, with its admired achievements in research and education, was a major inspiration when a list-based system for general practitioners was introduced in Norway in 2001.
Since Margaret Thatcher’s fund holding, the various British NHS reforms have been watched and viewed with interest and some anxiety among Norwegians, who believe in the virtues of an equitable health service provided according to need and not according to wealth. Nevertheless, the latest white paper by the Cameron coalition government, «Liberating the NHS», may undermine these ideas.
The purpose of this presentation is to examine our common ideals for health care, where these ideas came from and what impact the suggested British reforms may have on Norwegian health care.
Each nation needs to develop its own memory of how solidarity systems were in fact developed through collective struggle.
Julian Tudor Hart, 2007
This quotation by Julian Tudor Hart sets the stage: The Norwegian welfare state is not an evidence-based project, nor have the founding ideas for a comprehensive and publicly financed health care system come out of the blue – as pure ideas. Rather, these social institutions were the result of longlasting political processes with conflicts and reconciliations.
Over the years, I have come to be increasingly impressed by the wisdom, struggles, reconciliation, discipline and will not to resort to internal violence, which has become a hallmark of the Nordic countries over the last century. One great ideal coming out of these processes is equity, equality, egalité, maybe more so than in any other democratic country in the world. Particularly in the years after the Second World War, most policies and political parties have – more or less willingly – promoted ideas and practices aimed at the redistribution of wealth by means of taxation, by extensive social security and welfare legislation, by means of collective institutions and universal welfare, by means of free education and free health care for everyone and through strong labour inspection laws.
This is when I understand the famous British historian, Arnold J. Toynbee (1899–1975), who once stated: «Civilization is a movement and not a condition, a voyage and not a harbour». The rise and fall of civilizations was his preoccupation, which reminds us that any civilization is on the move, from somewhere – towards somewhere. And so are the Nordic welfare states and their health services. The questions are: So what is the direction? From where did the visions come? What is worth defending, and what needs to change?
Liberating the NHS?
The reason for us to take up the topic is the recent white paper by the David Cameron coalition government released in July of last year, named «Equity and excellence: Liberating the NHS» (1).
I have to admit that I had to look twice: «Liberating»? and «Equity and excellence»? Big words, and the following text no less in its grandeur: «… The vision builds on the core values and principles of the NHS – a comprehensive service available to all, free at the point of use, based on need, not ability to pay.» This sounds like an echoing of the late Aneurin Bevan, announcing the original 1948 NHS reform:
Equity and excellence: Liberating the NHS
Published: 12 July 2010

Figure 1 – From the Department of Health web pages, announcing its white paper in 2010.
The NHS White Paper, Equity and excellence: Liberating the NHS, sets out the Government’s long-term vision for the future of the NHS. The vision builds on the core values and principles of the NHS – a comprehensive service, available to all, free at the point of use, based on need, not ability to pay. It sets out how we will:
put patients at the heart of everything the NHS does;
focus on continuously improving those things that really matter to patients – the outcome of their healthcare; and
empower and liberate clinicians to innovate, with the freedom to focus on improving healthcare services
On July 5th there is no reason why the whole of the doctor-patient relationship should not be freed from what most of us feel should be irrelevant to it, the money factor, the collection of fees or thinking how to pay fees – an aspect of practice already distasteful to many practitioners…
On further reading, however, an entirely different picture emerges, making the department’s announcement sound like Orwellian New Speak. I realized that my anxieties were shared by others, as well as friends and colleagues in the UK, all of whom reported that they were no less than shocked. In their election campaign, the Conservative Party had presented themselves as defenders of the NHS, which I have learned is the ever discussed but most loved British public institution. «No more reforms» is what was said after a period in which the number of reforms allegedly matched the number of years since the conservatives introduced internal markets and the fund holding reform in 1991.
It took some time before the major medical journals really announced their stand on this. On January 29th of this year, I first read the Lancet editorial, «The end of the National Health Service», without questioning it (2). Next, a BMJ editorial on the same date directly addressed the UK Secretary of State for Health, Andrew Lansley, the minister who presented the white paper: «Dr Lansley’s monster: Too soon to let out of the lab» (3), which was illustrated by a not very nice-looking Mr. Hyde monster, and introduced the text like this:
What do you call a government that embarks on the biggest upheaval of the NHS in its 63-year history, at a breakneck speed, while simultaneously trying to make unprecedented financial savings? The politically correct answer has got to be: mad.
Some years earlier I had quite accidentally come across an interesting but rather disquieting book in a London bookstore, warning about an impending privatization of the NHS, by someone named Allyson Pollock (4). I bought it and was no less alarmed at what seemed to be happening to the health services in the UK, with the public-private initiatives and all that. She has contributed considerably to the rising amount of critique, stating plainly in the BMJ that «the secretary of state for health proposes to abolish the NHS in England» (5). Allyson Pollock also appears in writing and movies on the Internet pages of what is now called KONP, a grass-roots movement to «Keep Our National Health Service Public» (6), which is a big resource for critical books, pamphlets and video presentations. And of course, for those who know where to look for the long story of the NHS, Julian Tudor Hart’s book from 2006 was a revelation, and no less so with its updated version in 2010 (7). It is already clear that the British Medical Association is strongly against the reform, as are the Royal Colleges.
To a foreigner, it is hard to see how a government white paper can possibly survive such a massive resistance. Somehow though, the bill seems to have continued on through Parliament under the umbrella of Cameron’s «Big Society», which, by the way, some Norwegian politicians have taken an open interest in since it also implies decentralization and possibly less public spending (8).
Bridges to Britain
So yes, there is indeed still a strong link to Britain in relation to science, culture and politics. When general practice was emerging as an academic discipline in the 1960s and 70s, the Norwegian founders were most of all looking to Britain and the Royal College of General Practitioners (9). I have learned that my colleagues in other medical disciplines have had similar experiences related to British hospitals and research institutions. To Norwegians, Germany was out after the war.
As a young assistant professor of general practice with a group of medical students in 1980, I shall never forget the inspiring meetings with the RCGP people when visiting the headquarters at Prince’s Gate 14, which is a wonderful building south of Hyde Park. On a later occasion, I was asked by the BMJ editor to contribute to their special issue in 1998 to celebrate the NHS at 50 (10). I had to look deeper into the founding ideas of the NHS, and I guess this is when I started to learn about the Beveridge Commission and the brave moves by the post-war health minister, Aneurin Bevan (1897–1960), and Labour’s NHS reform (11).
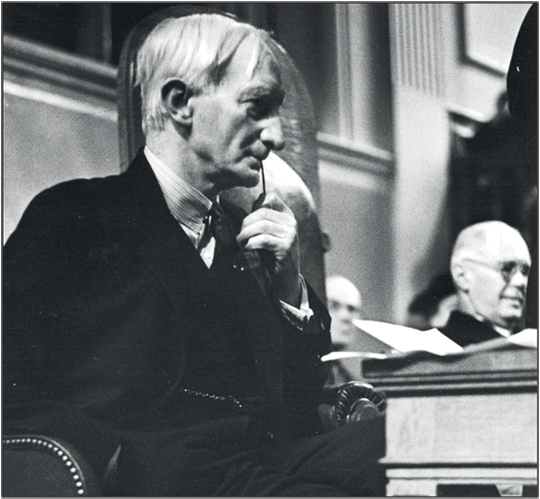
Figure 2. Lord Beveridge.
I have to admit that it feels overly ambitious to present my interpretations of British social history in front of British natives, although I shall try to make some remarks on how I think Britain’s intellectual and political life have made an impact on post-war developments in Norwegian health care and social politics.
A brief history of health care for all
When Norwegian social history is told, reference is often made to the social consequences of late 1800s industrialization and urbanization, and to the political moves made by the German Chancellor Otto von Bismarck (1815–1898) in the 1880s. A common notion is that his groundbreaking reforms to implement the first state-based social security reforms were not generated from altruism or great humanitarian values, but rather strategic moves allowing him to curb the rising power of the revolutionary labour movement.
Any enthusiast for the computer game Civilization knows that when there is social unrest among poor peasants, or a revolution by hungry workers looms, «building a temple», means to either give the poor some social reforms or build a church. This helps to restore social stability. In other words, several objectives, but Germany and Norway as well, received the first state-based social security legislation and labour protection laws.
There may be similarities in different political processes during the Second World War. One key question could be: What motivated Winston Churchill and his war cabinet to set up a grand commission for social reforms in 1941 – under the leadership of a former colonial bureaucrat William Beveridge (1879–1963) – at a time when Hitler’s bombs were still raining over London and no one knew for sure how or when the war would end?
The Second World War was not only about battles, bombs, tanks, invasions and brave collective resistance against the Nazis. It was also a war of ideas, a fight over visions for the future. This fight took place not only between nations, but also inside each country. One of Hitler’s tempting visions was his social programmes with work for all and campaigns for education, good health and health services for all – all Aryans at least (12). The Dutch primary health care system, with a general practitioner – a huisarzt – for everyone, was implemented by the Germans during the war, which was actually the first list-based system for general practice in Europe, and they still have it.
The challenge was not only from the right – from the social order and hygienic visions of the Nazis. There was a challenge from the left as well. We must remember that social conditions for the working class in Europe under the economic recession of the 1930s were bad, very bad. Socialist and communist ideologies provided inspiring ideas for social justice and visions for a better life. The Spanish Civil War from 1936 was a formative event for an entire generation of youth in Europe.
During the initial phases of the subsequent Second World War, there were questions of war morale. It was by no means certain that the poor working classes of the allied countries would sacrifice their lives in defence of a society with immense class differences, unemployment and social injustice. Visions of a socialistic revolution were part of the political scene.
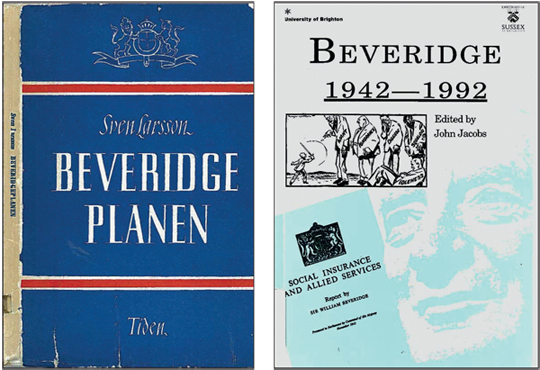
Figure 3 – The Beveridge Report: Facsimile from the Swedish translation in 1943, and one of many publications celebrating the Commission’s 50th anniversary.
We can imagine that memories of the Russian Revolution in 1917, when poor Russian soldiers turned their guns towards their own ruling class and the Tsar, were causing unpleasant dreams among the British aristocracy, even into the initial years of the war. Why fight and die for the benefit of the upper classes? Rather, the revolution – or Hitler – would promise them a brighter future. Churchill and the British upper class must have had plenty to worry about. To Norwegians, these conflicts are vividly brought to life in the popular British TV series «Foyle’s War», which features crime stories from southern England with an impressively detailed social background (such as Inspector Foyle’s assistant driver, Sam, leaving a restaurant table, and her date, because she disliked his disapproval of the Beveridge ideas).
If the computer game Civilization had been there for Churchill and the Allies at the time, there would be one clear message for survival and success. Do something to boost morale: create a vision for a better future, a common future, something worth fighting or even dying for. Freedom was a great slogan, but hardly enough for the working class and the poor. Adding social justice to the vision would certainly help.
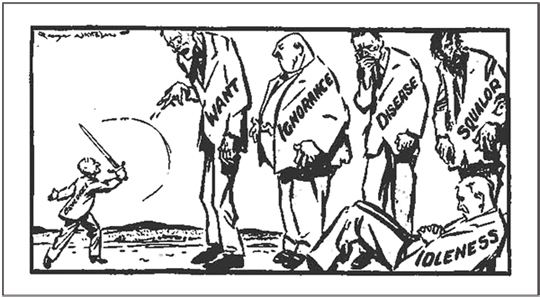
Figure 4 – Contemporary cartoon, showing Beveridge fighting the five evils.
This could be one answer to my previous question: Why did Churchill and his war cabinet bother to set up a commission for social reform during the battle of Britain? However, the answer is probably more complex. It seems as if Churchill was reluctant to accept the wider implications of the Commission’s report, as social policy lecturer John Jacobs writes in 1992 (13):
Beveridge had handed the wartime Coalition Government a Plan which could have revitalised the nation, boosted morale and enlisted the energies and commitments of the people in the war effort. Had they understood the effect it had on the public they would have embraced it with open arms and set about implementing the main proposals. But Churchill, far from welcoming the Report, set about trying to put the genie that Beveridge had released back into the bottle.
The Report was released in 1942 right after the battle of El Alamein, a time of emerging optimism for the Allies. «Legend has it», writes John Jacobs, «that a queue a mile long formed outside the Government Stationary Office in Kingsway; it sold over 635,000 copies, and the press and public were nothing short of ecstatic in its praise». A large number of copies were brought illegally behind the German lines as proof of the Allies’ promises for a brighter future. A copy was even reported found in Hitler’s Berlinbunker after the fall of the Third Reich. In United States as well, it created a lot of optimism among workers and the poor. Why and how the Report was silenced in the US is another, and quite interesting, story (14).
The Report, which can be found on the Internet today as well, is rather technical, but presents strategies to fight the «five evils» of want, ignorance, disease, squalor and idleness. In Brian Abel-Smith’s words (15):
The report advocated family allowances, a free health service and full employment, and that all social insurance benefits should be at flat rate and at subsistence level with the aim of abolishing poverty. …
And, importantly to our context:
… The report had a major influence in other countries by setting a much more ambitious agenda for social security than had generally been accepted before.
More generally, the Commission’s report could be seen as a strategy for overcoming class conflicts. The aristocracy and the rich would have to give up some of their privileges to join in a social project aimed at providing more social justice for all. A stronger public sector financed by progressive taxation, thereby providing free education and free health services for all, even for children of the working classes, seemed necessary. A grand social contract, promising a brighter future for the poor once the war against Hitler was won, was something worth fighting for.
The outlines of the post-war welfare states had been created. In contrast to its position during the Spanish Civil War, churches and clergy in allied countries were now more sympathetic to the working-class movement, and to economic and social reforms. The reinvention of the word «welfare state», previously suggested in 1880s Germany, was possibly done by Archbishop of Canterbury William Temple (1881–1944), who in a famous speech endorsed the report by contrasting the visions of a «welfare state» with the German «warfare state».
Norwegian politicians and intellectuals in exile in London were certainly part of those political discussions. And the ideas had an impact on the political agenda in Denmark and Sweden as well. The Report was actually translated into Swedish during the war in 1943 (16). The charismatic Norwegian Surgeon General Karl Evang (1902–81) was among those influenced by the new ideas. As a medical student, I heard him lecture enthusiastically about the prospects of improved population health in the new kind of society: The welfare state, with free health care for all. And with state-based social security programmes to maintain purchasing power among the unemployed in case of recessions, to avoid the earlier crises of capitalism – welfare, stability and prosperity in one package! The post-war welfare programme of 1948 in Norway (Folketrygdmeldingen) was almost a blueprint of the ideas from the Beveridge Commission (17).
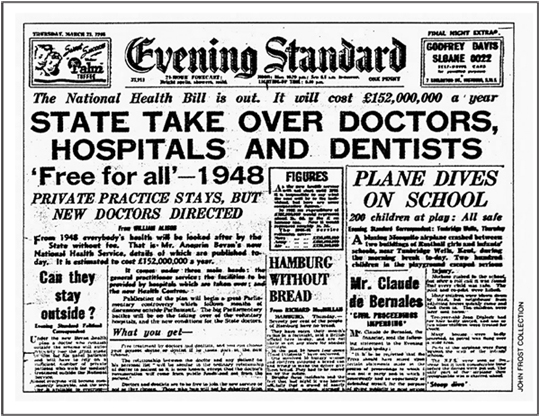
Figure 5 – The Evening S0074andard announcing the NHS reform, July 5, 1948.
The socialist revolution had been cancelled. The modern welfare state would make us all more equal, a peaceful social revolution without the hassles and dangers of a socialist revolution. Education and health care had to be a public responsibility, a human right for all that was sheltered from the injustices of the market. No longer should health care be a marketed commodity (18).
Most of us know the rest of that story. Britain got its National Health Service on July 5, 1948 (10–11), which was a dramatic and brave move by Secretary of State Aneurin Bevan in the post-war Labour government (11). «A new path entirely» for health care and welfare was his vision – and he could not conceal his disappointment with those medical doctors who opposed the reform out of pure business- and self interest he alleged. I later met some of those dissident doctors who fled to Australia, now regretting that they had failed Bevan. They were too late to see the braveness in the Beveridge visions of welfare state institutions.
By many measures, the NHS must have been a tremendous success. In the late 1980s, the NHS provided equitable health services to all British inhabitants at a cost per person slightly below the cost of just the administration of American health care (14). And then – as now – with millions of American people still uninsured. In my understanding, the problems of the NHS emerged when underfunding was obvious, in spite of it being very efficient. Tax-based financing is always challenged by the private market’s «willingness to pay».
With their universal welfare-for-all policies, the Nordic welfare states have also proven to be a success, both economically and socially (19). And importantly, the frameworks of the welfare states had been created «before the oil». Otherwise, when foreigners look to Norway or the Nordic countries with some admiration for the welfare legislation and universal free health care, their usual response is «it must be the oil». It was not. It was about ideas.
Implications for health care today
This story about why education and health care were removed from the market is largely forgotten in Norway – and I guess in the other Nordic countries as well. We assume that social structures are there to take care of us and our patients on equal terms, whenever it is needed. And for many years, we largely ceased to worry about social injustice or inequalities in health.
The common political consensus was that social classes had gradually disappeared – or merged – and that equity was achieved, and we were all becoming more equal. It is a nice vision, and to some extent it is true. There was indeed a trend towards more income equality during the post-war years, which is probably why the Nordic countries are still in the top rankings on many desired indices of health and health services (18, 20). However, since the 1980s socioeconomic differences in income and living conditions have gradually increased in all the Nordic countries, with Norway rising at the fastest rate, more precisely with a turning point in 1989 (Central Bureau of Statistics data, 2011). In many areas, the market has been striking back and challenging the health services (20), as well as the distribution of wealth. To quote Julian Tudor Hart again: «Greed is a powerful, but dangerous fuel to social machinery».
When epidemiologists started looking at health differentials in Norway in the 1990s, a worrying pattern emerged: The disparities in health and gradients in mortality were clearly increasing between the best-off and the worst-off, which was particularly easy to demonstrate among men (21).
The present Norwegian government has given this issue a high priority. Five years ago a white paper was presented to the Norwegian Parliament, the Storting, on «Strategies to reduce social inequalities in health» (22).
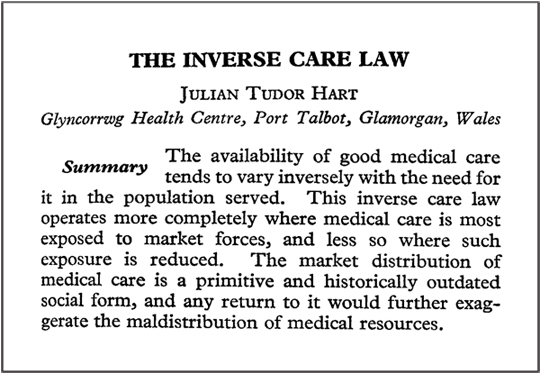
Figure 6 – Facsimile of the 1971 Lancet paper, well-known to anyone concerned with equitable health services.
From a public health point of view, it is a rather great document, if documents can move the world. The white paper acknowledges the importance of looking at the «causes of the causes» for inequities, and announces initiatives in many sectors. It also challenges us in the health services to look more closely into whether the ideals of equity in health care are as real as we want to think.
The white paper makes special reference to the seminal paper by Julian Tudor Hart from the Lancet in 1971, presenting evidence for what he found to be an «Inverse care law» that was more or less visibly influencing the health services, (23). It is about the tendency for the health services to be worst for the people most in need of them. It has been a long time since this paper was published, although its message has gained increasing importance, as market mechanisms are being re-introduced into the health services in our part of the world without much concern about their side effect: increasing inequalities in the health services (20,24). The inverse care law is not a law of nature, as Julian Tudor Hart has emphasized. It is a description of what happens when health services are exposed to market mechanisms (25).
Why worry?
The impending reforms – or «the end of « – the NHS, if this is the prospect, will certainly be a major challenge to the Norwegian and Nordic health care systems. I think we have to raise a broader discussion about how neo-liberal politics and economic corporate interests can erode, or simply undermine, the principles of public funding, solidarity, comprehensiveness and equity. Under the pressure of economic globalization and market forces, health care is undergoing processes of «commodification» even in our countries, turning health services into commodities with price tags, patients into customers and doctors into commodity producers. In turn, this offers opportunities for big business to enter this huge, and up until now, largely uncommodified public sector. «Immature markets» have always been a challenge to big business.
Or we may look at it more ambitiously – as an editorial in the Scandinavian Journal of Primary Health Care did some years ago (26): «… an ambition to bring a message more forcefully to the world… that we have developed health care models worth looking at.» We used to look to Britain, to the NHS. Soon, we may have to resort to a fresh version of Franklin Roosevelt’s «look to Norway» – or rather, «look to the Nordic countries». In spite of the problems and challenges, and potential for improvements, our health services are basically there when needed – for all. We hope this will be the case for the NHS as well. But we will certainly, once again, keep our eyes on what happens to the NHS in Britain.
Literature
Department of health. Equity and excellence: Liberating the NHS. White paper 12th July 2010. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_117353
Editorial. The end of our National Health Service. Lancet 2011; 377: 353.
Delamothe T, Godlee F. Dr Lansley’s Monster: Too early to let out of the lab. BMJ 2011; 342: 237–8.
Pollock A. NHS plc. The Privatisation of our Health Care. London: Verso, 2005.
Pollock A, Price D. How the secretary of state for health proposes to abolish the NHS in England. BMJ 2011; 342: 801–6.
http://www.keepournhspublic.com/index.php
Hart JT. The political economy of health care. A clinical perspective. Bristol: The Policy Press, 2006. Second edition, new subtitle: Where the NHS came from and where it could lead, 2010.
Homburg TB. Vil lære av Storbritannia (Want to learn from Great Britain). Aftenposten 5th May 2011, p 4.
Evensen SA, Gradmann C, Larsen Ø, Nylenna M (red.) Allmennmedisin som akademisk fag (General practice as an academic discipline). Michael Quarterly 2009; 6:11–126.
Westin S. The NHS’s 50th anniversary: A great leap for humankind? BMJ 1998: 317: 49–51.
Portillo M. The NHS’s 50th anniversary. Something to celebrate. The Bevan legacy. BMJ 1998; 317: 37–40.
Sørensen Ø. Solkors og solidaritet («Sun-cross» (Norwegian nazi-symbol) and solidarity). Oslo: Cappelen, 1991.
Jacobs J. An introduction to the Beveridge Report. In: Jacobs J. (ed.) Beveridge 1942–1992. Papers to mark the 50th Anniversary of the Beveridge Report. London: Whiting & Birch Ltd, 1992.
Himmelstein DU, Woolhandler S. NHS at 50: An American view. Lancet 1998; 352: 54–5.
Abel-Smith B. The Beveridge Report: Its origins and outcomes. Int Social Security Review 1992; 45: 5–16. http://www.blackwell-synergy.com/doi/abs/10.1111/j.1468–246X.1992. tb00900.x.
Larsson S. Beveridgeplanen – i sammandrag. Stockholm: Tiden förlag, 1943.
St.meld nr. 58 for 1948: Om folketrygden. (White paper to the Norwegian Parliament) (Storting).
Nylenna M. Norway’s de-centralized, single-payer health system faces great challenges JAMA 1995: 274: 120–4.
Westin S. Welfare for all – or only for the needy? Lancet 2008; 372: 1609–10. http://www.thelancet.com/journals/lancet/article/PIIS0140–6736(08)61666–9/fulltext
Wilkinson R, Pickett K. The spirit level: Why equality is better for everyone. London: Penguin, 2009.
Westin S. The market is a strange creature: family medicine meeting the challenges of the changing political and socioeconomic structure. Fam Pract 1995; 12: 394–401.
St.mld. nr. 20 (2006–2007). National strategy to reduce social inequalities in health. White paper to the Norwegian Parliament (Storting).
Hart JT. The inverse care law. Lancet 1971; i: 405–12.
Hart JT. Commentary: three decades of the inverse care law. BMJ 2000; 320: 18–9.
Hart JT. Two paths for medical practice? Lancet 1992; 340:772–5.
Sigurdsson JA, Stavdal A, Getz L. The Nordic Congress of General Practice: A gateway to a global treasure? Scand J Prim Health Care 2006; 24: 196–8.
General Practitioner and Professor of Social Medicine
Department of Public Health and General Practice
Norwegian University of Science and Technology (NTNU)
Trondheim, Norway
steinar.westin@ntnu.no
