What happened to Latvian health care 1991–2004?
The hospital issue
Around 1991, something special occurred in Latvian hospitals. People at the top of the management started to think in another way than they had done before. They started to count money. And it was especially the expenditures that caught their interest, the efficiency of the resources used. In the beginning it was the cost of drugs, but gradually this new interest in money also was expanded to cover the use of lab-tests and other examination and treatment methods. Health care, in a way, had been exempt from budget analyses because of the complexity and the variety of values involved, but now reforms were asked for – which still have not been completely carried through.
Formerly, only little attention had been paid to the costs incurred by the patients, because the health care system simply was there. The services were state run and finances were not an important part of the management principles.
By 1994 sickness funds were established, and they started to purchase medical services from hospitals and policlinics. From now on all health care institutions had entered business.
The buying of health services by the sickness funds indeed meant the start of health care reforms in the new Latvia. Health care got a price in a quite new way. However, the Latvians had a constitutionally settled right for getting health care when needed. Now the government indeed fulfilled their obligations when it came to words, but not in terms of money. The sickness funds had been allocated money for health care, but it was not enough to meet the prices of the services offered by the hospitals. There was a gap, even when patient co-payment was included. For a while, this gap could be filled by reorganising hospital work so that it became more cost efficient, but there was a limit to what could be achieved that way. A gap persisted, and with it a problem which has not been fully solved even in 2005, in spite of several attempts at solutions that have been launched.
Another point to be reviewed was that in hospitals, remuneration mainly took place as giving a sum for each day a patient occupied a bed. Salaries were still low. Due to under-financing by public money, some hospitals tried to find ways to increase their incomes. As an example, often hospitals near each other bought expensive equipment which easily could have been shared, in order to offer specialised diagnostics and treatment. At the bottom level, however, no better service emerged from the amelioration of their finances.
Hospitals/beds |
2000 |
2001 |
2002 |
Number of hospitals |
142 |
140 |
129 |
Number of beds (per 10 000) |
87,3 |
82,3 |
77,0 |
Physicians |
2000 |
2001 |
2002 |
Number of physicians (total) |
8134 |
7744 |
7921 |
Number of physicians (per 10 000) |
33,6 |
33,0 |
33,8 |
Nurses |
2000 |
2001 |
2002 |
Number of nurses (total) |
14 934 |
14 663 |
14 610 |
Number of nurses (per 10 000) |
63,1 |
62,5 |
62,3 |
Visits |
2000 |
2001 |
2002 |
Number of visits (in millions) |
11,4 |
11,2 |
10,7 |
Number of visits (per capita) |
4,82 |
4,80 |
4,54 |
|
1991 |
1995 |
1998 |
1999 |
2000 |
Hospital beds |
135,9 |
112,2 |
92,9 |
88,5 |
85,2 |
|
2001 (%) |
2002 (%) |
Diseases of circulatory system |
17,2 |
15,7 |
Injuries, intoxications and consequences of external causes |
10,6 |
11 |
Diseases of digestive system |
9,4 |
9,5 |
Tumours |
9,2 |
8,3 |
Diseases of genitourinary system |
8,3 |
6,8 |
1998 |
1999 |
2000 |
2001 |
2002 |
|---|---|---|---|---|
15 606 |
15 344 |
14 934 |
14 663 |
14 610 |
The same distortions could be seen in a primary health care setting. Again an example: Each doctor, on the basic level, had a virtual sum for refundable medicine and for examinations. This sum could not be exceeded, if so, the doctor had to pay from his own pocket, as her or his revenues then would be deducted with the excess of expenses. Protests of course were heard and the interest by journalists awakened. But the hunting for scapegoats caught the wrong game. It was not the single doctors or the single hospitals that were to blame; it was the state which did not pay for what it had promised, i.e. the gap between expenses and funding. Problems had been delegated downwards to those health care providers who fronted the public, but who had no influence on the system by themselves.
And what about the impact on people’s health? The deplorable fact was that life expectancy dropped, and other health indicators worsened, but to assess the meaning of each and every one of the possible destructive factors, where cutbacks in hospital services was only one of them, is not easy* See discussions in Cockerham 1999.. Yet the grass-root fact was that a normal hospital stay, which in Soviet times had been, say twenty days, had dropped substantially, without any efficient primary health care services to make up for it.
Would an upgraded primary health care system be better?
Riga municipality was the first one in Latvia to introduce a primary health care system in 1996. This was followed by a law on physicians’ practice which opened up for private practice offered by physicians, a system familiar to all in the Western world, but till then uncommon in Latvia. Only then was private practice for physicians allowed to expand. As independent contractors, selling services to the sickness funds, general practitioners could employ assistant personnel and set up an efficient way of working. Of course it became difficult to assess the health effect of this new system. Some statistics were made based on prescriptions given away by family doctors, referral documents etc., but results were not conclusive.* See: Health in Riga. In fact, there was some protest that needed to be heard: Formerly, patients could choose to go directly to a specialist. Now a new level had been put into the system, a new step to overcome, an independent contractor who operated with waiting lists, only to do paperwork which only generated new waiting, and the doctor even cashed in money for this backward step in the service!
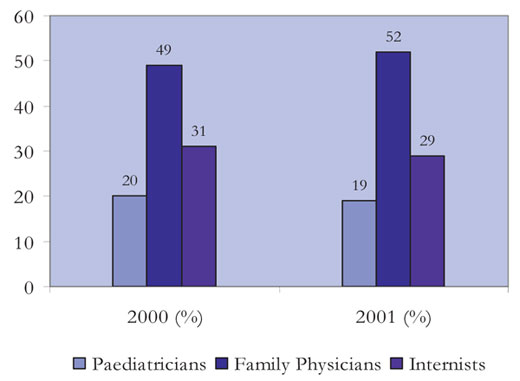
Structure of physicians in primary health care
Number of family doctors
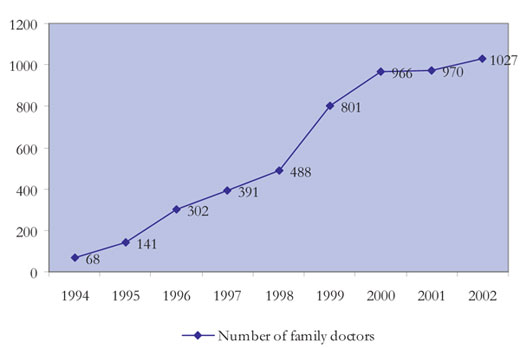
Earlier, the primary encounters between people and the health services when demands arose, was usually with district internists or paediatricians in policlinics, or specialists. The new system implied that the primary care physician could be met in his office or in a house-call situation. In the old days, people rang the policlinic or to the doctor’s office, requesting a home visit, and at the end of the day the doctor would come. In the new situation, when finances improved, and – not least – when a telephone had become available to everyone, requests for house calls had soon exceeded any capacity on the side of the practitioner. A selection had to be done, advice given by telephone to those where this seemed appropriate, and those better examined in the office asked to come there. Did the new system, as a side effect, shape an image of arrogant doctors?
Freedom – also from disease prevention?
Latvia was the first republic in the Soviet Union to introduce the KASMON, a computerised system requiring all inhabitants of Latvia to give health information to a common database* See Kanep & al. 1988.. Under a totalitarian rule this large scale project was possible to implement, and soon coverage had attained a high level, and data for most of the population became available for preventive purposes. As discussed by Cockerham (1999), emphasis traditionally had been laid on secondary prevention, and here the new computer based system had definite assets. PAP-smears, x-ray findings etc. could more readily be followed up than before, and in fact some important health parameters were influenced in the right direction, such as for tuberculosis and certain cancer types. Under democracy, this was not that easy anymore. To many, freedom also included freedom from totalitarian paternalism, also when it came to health.
In Soviet times there also existed a system of so called «dispenserisation» for certain categories of patients. This meant mandatory annual follow ups. The health personnel had to actively get in contact with these patients to examine them and see to it that the treatment was followed as prescribed. Rheumatic diseases, hypertension, peptic ulcer, chronic obstructive pulmonary disease patients belonged to these categories. After 1991 this follow-up system was discontinued and it faded away, as the responsibility for health was handed over to the patients themselves. Perhaps this was a misinterpretation of the benefits of democracy, but anyway, a system for preventive medicine which had proved to be useful, was not maintained. The pendulum had swung over to the other extreme. Positive health effects inherent in Soviet paternalism 1 See Kanep & al. 1988. were thrown away, and so were also the health gains connected with it. In the end of the 1990’ies it was attempted to reintroduce preventive schemes, but then the initiatives were met with lack of resources.
Diptheria in the 1990’ies
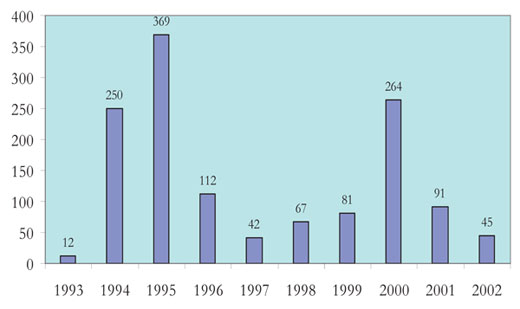
(Note the two epidemics!)
The Soviet Union had a good reputation when it came to vaccination against infectious diseases. Controls were heavy to secure that plans were followed. It is also a medical fact that the effect of vaccination in a population is at its best when as many as possible are vaccinated. This means, that if the percentage of vaccinated persons is lowered, the general protective effect also will be lowered. During the Soviet period much of the vaccinations were carried out in schools. The schools had nurses and doctors, and the pupils were vaccinated in the school health department’s premises. By the late 1990s resources allocated for school physicians disappeared, and the school nurses had to continue by themselves, which later was regarded as medically inappropriate. Then it was claimed that the nurses’ offices did not comply with the requirements for vaccination rooms, and the solution at hand was to discontinue vaccination at schools.
In the old Soviet system a special responsibility for the health of children was placed on the district paediatricians. Now these had to be retrained to become general practitioners, or the general practitioners had to take over the care for the children. Allegations were heard that the training programmes simply did not provide the necessary knowledge and the skills required to take care of children’s health in an optimal way.
Did the pensioners rebuild Latvia?
The care for the elderly is a central part of the health care in most Western countries. Even in countries where life expectancy is below a desirable level, the numbers of elderly people is substantial. When normal retirement age is low, such as in Latvia (1991: female 55, male 60; after pension reform gradually increasing to 65 for both sexes), this adds to the numbers of persons needing public support for subsistence and health care.
In Latvia, there was a large group of the population sixty years and older, by 1989 463109 or 17,4 % out of the total of 2666567.* Latvian Health Statistics 1990. These people had spent their working years in the Soviet period and they had been looking forward to a pension which would allow them a decent life, as circumstances permitted and according to the prevailing standards. 1991–1993 there was a monetary unrest, leading to a hyperinflation on the annual level of 900–1100 per cent. Prices were also rising in real terms, so when the pensions remained on the old scale, it became simply impossible to live from the pension. Those who had no children or other relatives or benefactors to support them, had a really hard time. The lack of proper health services, which in addition had been for free before, added to the problems for health and health care.
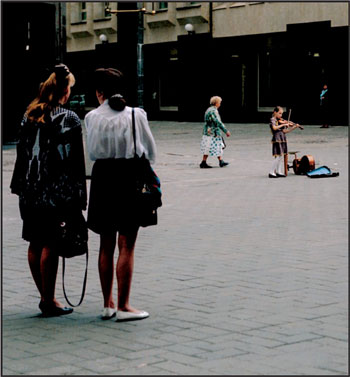
Women from four age groups on Kalku street in Riga 1995* See Larsen 1999..
Pension reforms were carried through, but anyhow, conditions for pensioners have been deplorable. Because many factors have changed simultaneously, it is not so easy to compare pensions 1991 and 2004, but still, if pensioners feel a bit abandoned by the state, they could be right.
In another perspective, when the State held back an increase in pensions and used available funds for other purposes, it can be said that the sacrifices given by the pensioners after Latvia’s independence were used for other national improvements.
Sharper formulated: Old people who had endured the meagre Soviet years and drawn the baseline for the rejuvenation of the Latvian society, had to pay a substantial price for the progress primarily enjoyed by their successors.

Riga 1994, still with an Eastern look.
