The medical reports from the district physicians – an indispensable source to the Norwegian medical past
Michael 2005; 2: 218–35.
1803 – The year of birth
According to a circular by December 20th, 1803 from the Medical College in Copenhagen, all County Governors of the realm were told to instruct all «in his district employed country physicians, district surgeons and other practising doctors» to submit annually «Intelligence on the various items, that are to be listed below; such reports shall forthwith and without delay be sent to the Medical College in Copenhagen, and from there, through the Danish Chancellery, to be presented to the King (1) (fig1).
Fig 1. Governmental circular of December 20th, 1803 on the introduction of mandatory medical reports.
Thus the foundation was laid for annual, mandatory reports from the doctors to the central health authorities. These measures were strengthened as early as 1807, and several times thereafter. In Norway, it lasted till 1984, when the institution of district physicians ceased to exist.
Before 1803 it was primarily the task of the clergy both to report to the County Governor (as superior authority) on epidemics, but also to take measures against contagious diseases. At that time, such measures were information to the public, often from the pulpit or at the church green, and the distribution of medical drugs. This was addressed in some detail by a decree of April 17th, 1782 (2). Here the public was obliged to report to the local vicar of serious diseases or other conditions that were considered to be dangerous or contagious. At the same time, the estate owner, the County Governor or the farmer «promptly get the county physician or other capably examined doctor, to explore the disease and ordain the required drugs against it». If the doctor had discovered a contagious disease, he was instructed to «promptly make a meticulous report to the Medical College».
This ordinance applied to Denmark, but in practical terms to Norway as well as far the central role of the vicar was concerned. In the regulations of 1803, new directions were introduced that applied to both countries. The reporting requirement was significantly enhanced to «everything that pertains to the public health care». The reasons presented for this reporting requirement in the need of the authorities «to be capable of, prescribe the most adequate preventive measures towards the most regularly present diseases». Or, as we would have put it today: The decision makers’ need for updated information from a superior professional and supervisory body on public health.
Central health authorities
The Medical College was established in 1740 as an advisory body to the authorities. In 1803 the political development indicated that this institution was replaced by a college within the central government, i.e. a body of public administration. Its functions were approximately those of a directorate, and it sorted under the Danish Chancellery, or Ministry of the Interior (3). In 1809 the state of war led to the establishment of a distinct Norwegian health college («Sundhedscollegium»). In 1815, after the separation of Denmark and Norway, these functions were transferred to a medical agency that was placed in different ministries till 1891. Then, the medical reports were submitted to the newly established national board of Health. This body was placed outside the ministry and was headed by a medical director. To day the central health management consists mainly of the Ministry of Health with two agencies: a National Board of Health, a supervision authority; and a Directorate of Health and Social Affairs.
The underlying conditions for the reports
The reason why this process took place from approximately 1770, was to a large extent the recognition by the autocratic state that public health was a public responsibility, at the same time as the need of the government to exercise control was increasing. This, in its turn, was linked to the political philosophy of that time – mercantilism – in which a healthy population was a prerequisite for a strong national state. In order to be able to act politically it was necessary with more information, i.e. on the health conditions of the domain. This recognition was made more pertinent and strengthened by the increasing frequency of contagious diseases, in Norway by «radesyke» (traditionally viewed as a tertiary form of syphilis) as well. It is worth noting that such gathering of information built on a certain tradition. In that respect we can refer to the first health law of the country, «Ordinance on Medics and Pharmacists» of 1672, section 9: «Medics, everywhere in Royal domains and land shall annually, or when circumstances occur, communicate with the Dean of the Faculty in Copenhagen whatever might appear remarkable or peculiar within medicine or nature..»(4). To what extent this obligation was followed up is uncertain, but it is an indication of the emerging interest in public health and responsibility for the welfare of the people on the part of the Crown.
Henceforth, an information system within the public administration represented nothing new. For example, as of the 18th century both the clergy and the local magistrates had a duty to report, and somewhat later came the introduction of quintennial reports of the County Governors. The gathering of information, that was so typical for the Era of Enlightenment, i.e. the 18th century, found its expression i.a. in the so-called topographical scripts. The best example of that in Norway is the priest from Sunnmøre Hans Strøm’s «Physic and economic description of the court district of Sundmør» from 1762 and 1766. In his publications he also included problems of public health. His writing was known among his contemporaries, and among other, the Chamber of Interest (the equivalent of the Ministry of Finance) in Copenhagen wanted to use his knowledge as a foundation for its work (5).
It was therefore a number of conditions that led to a strengthened health service in the country. One of the measures was the appointmens of several public physicians and establishment of hospitals in the counties, effectively for veneral diseases and «radesyke». The introduction of annual and mandatory medical reports was an equally important measure, as it meant a significant means of assuring the quality of the knowledge of the central authorities on the state of diseases within the population and on the public health. The modernization of the health services that thus took place, created the foundation for the arrangements of our times, and it is not hard to say that the fundamental elements in the construction of those days are about the same as today.The reports of 1804
The directive of December 20th, 1803 indicated that the first reports would pertain to the year 1804, that is, 200 years ago. The doctors were asked to inform on seven areas within health and health services:
« 1. Which diseases that have raged the most, particularly smallpox, itch, veneral diseases, and, in Norway, «radesyke».
2. Which of these that may have been caused either by the nature of means of nutrition or by the lack of such.
3. The progress of vaccinations .
4. Mortality, particularly among newborns and women in confinement.
5. The occurrence of unfortunate events
6. The number of practising doctors, and their conditions.
7. If there had been occasion to present complaints of quackery».
In addition, there were five questions concerning the «Pharmacist-institutions», which were under the supervisory responsibility of public doctors at that time.
The questions were relevant and reflected the public health problems of that time as they appeared to the central authorities. Smallpox and veneral diseases were particularly mentioned. This was not only because smallpox was a constantly reccurrent and feared disease with high mortality, but also because at this time there had been some initial vaccinations under public auspices. The authorities were well aware of Jenner’s work from 1798 and saw by that the opportunity of efficient prevention. Quick action was taken. Thus, the first vaccination in Denmark took place in 1801, and in Norway in March 1802, in Stavanger (5). The doctors were asked to report on the status of the vaccination, and seven years later, vaccination against smallpox was made mandatory (6).
As mentioned, it was in particular the increase in veneral diseases and «radesyke» among the population that caused the health reforms of the autocracy as of the 1770s and 1780s. This category of diseases, and particularly the «radesyke» has been addressed several times in medical historic literature, in Norway most lately in 2003 (5,8,9). It can be documented that veneral diseases – the distinction between gonorrhea and syphilis was not established until 1838 – was frequent among the population, and could be regarded as a common disesase. Early medical reports indicate this, and it has been confirmed from Sweden «that the veneral disease together with tuberculosis was the main health problem of the century» (10). The authorities in Denmark-Norway considered the conditions to be so grave that in 1807, through the District Governors and Bishops, distributed «Information concerning the veneral disease, its characteristics and consequences… for the information of the general public» (11).
The medical reports of 1804 have recently been published in a transcribed version by the National Board of Health (12). The original reports are kept in the National Archives in Oslo (13). They are not quite complete, as there are 27 reports from 13 out of 18 counties present. Regarding the authors, 11 doctors (county physicians) were graduates from a Faculty of Medicine at a university. 16 district surgeons submitted reports. Among these, four had no formal education while the remainder had studied at the Academy of Surgery in Copenhagen. In 1787 this education was made equivalent to a graduation from the Faculty of Medicine. Slightly more than 20 per cent of the authors were native Norwegians, the other were Danish and German (14). Their average age in 1804 was around 42 years. Among more established public servants, such as clergy and lawyers, the number of Norwegians was far higher. For example, only ten per cent of the parish vicars in 1800 were born in Denmark, the remainder were native Norwegians (15). One cause of this was that the medical profession within the domain was very small till the 1780s, and that the education could not take place in Norway before the establishment of the University of Christiania in 1811.
The structure of the medical reports
In the reports of 1804 there is a pattern that in many ways was preserved until 1984. They were drafted by the individual doctor, and reflected this doctor’s view of the public health within his district. These reports were then collected and considered into a context by a superior body before the final report was submitted to the Ministry. Here, they constituted the fundamental work of reference for the public health efforts of the central authorities. Whether it was the health college, the medicinal agency, the medicinal office or, later, the offices of the county public health officers and the National Board of Health, these evaluations and considerations were made by competent doctors and experts and thus increased the value of the reports (fig 2).
In the report of 1804 we have seen that the disposition is divided into two main parts. One was information on contagious diseases and other contemporary conditions or diseases; the other was mainly statistic records on health personnel and circumstances of mortality.
Fig 2. Cut from the original medical report of 1804 from county physician C. Lintrup in Hedemarken. National archives.
During the years between 1805 and 1813, the national archives only have sporadic reports, but as of 1814 they are complete, except from the years 1831–35. On August 24th , 1831 a «Letter from the Government Ministries of Church and Education» was sent to all authorized doctors in the country. This constituted an expansion and strengthening of «the ordered medical report», and replaced the guidelines of 1803. The doctors now had to express views on i.e. «which influence the weather might have had on the general health conditions». This was typically a question that pertained directly to the debate on causes of disease of that time.
It was more important that the doctors also were asked to describe people’s «way of life…which might be assumed as the cause of some of the diseases listed». This represented something new, and hereby the authorities assumed a modern, almost socio-economic view on diseases and their causes. One might readily assume that the increased documentation of the correlation between living conditions and diseases in the industrializing Europe had made its impact upon the medicinal office of the Ministry (16).
Gradually, the reporting requirements were expanded, both as far the statistical and the descriptive parts of the medicinal reports were concerned. After the passing of the new Public Health Act in 1861 the reports were standardized even further by the introduction of annual lists of cases and other statistics (17) (fig 3). This change implied a higher quality of the data, because they could be used to make comparisons between the regions, districts and parts of the country. The reports of practising doctors should now be sent to the district physician, who in his turn submitted his report to the County Governor. From there it was sent to the central health authorities in Christiania.
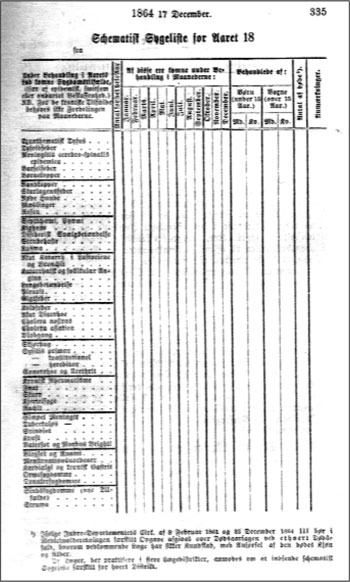
Fig 3. Annual list of diseases. Introduced in 1864.
«The State of Health and Medical Conditions in Norway»
As early as in 1815, the headline of the report from the health college to the Ministry got its permanent form: «Report on the State of Health and Medical Conditions in Norway». From 1853, they were printed as a part of Norway’s official statistics (fig 4). The reports soon found a form which remained fairly unchanged until our time. First there was a brief and general account of the health conditions of the land. A quote from 1853: «As it will appear in more detail from the following district reports the health conditions of the domain have been very good in 1853, clearly better than in the preceding year.» And as an example 50 years later: «The health conditions were by and large satisfactory».

Fig 4. The first printed «Report on the State of Health and Medical Conditions in Norway» (1853).
This introduction was followed by a numerical overview with comments on the conditions of diseases and mortality in the country, often distributed by districts, followed by a thorough analysis of the individual diseases, particularly the acutely contagious diseases, tuberculosis and veneral diseases, as well as infant and maternal mortality. There was also a presentation of statistics on causes of mortality. Psychiatric institutions and conditions concerning the «insane» were also described, and status on vaccinations was a constantly recurring item. Statistics on health personnel were also included.
Following this national overview, there was a corresponding presentation for the districts. The most significant difference is that here there is often a discussion on social conditions, e.g. poor economical ability of the municipalities, unemployment and hygiene among the population and of living conditions as risk factors for a prevailing disease, as well. Such comments in the district overviews were taken directly from de reports of the individual doctors.
Until 1930, selected reports of individual doctors were, partially or in their entirety, published as appendixes to the national reports. The first time that happened was in 1855, the district physicians Gerhard Brock (1813–59) in Inner Hardanger District and Holm Monsen (1812–88) in Midhordland District were the authors (18,19).
After the discontinuation of the institution of district physicians (or district public health officers) in 1984, the county public health officer took over as provider of information to the superior health authorities. Due to reorganizing, and henceforth changes in accountabilities and distributions of tasks within the central health authorities, the status of the reports within the chain of information became somewhat unclear, and still is.
Input to central political authorities is currently planned i.e. through so-called public health reports. These shall be drafted by the Ministry of Health and presented to Parliament. They are supposed to be published annually. The most important expert input to the Ministry comes from central health authorities such as the Directorate of Health, the Board of Health, the National Institute of Public Health etc.
The contents of the medical reports
It must be emphasized that the quality of the medical report was subject to variations, and that applied to the entire period from 1804 through 1984.
However, many of the reports were of a high quality both with respect to form and content, and shed light upon living conditions and development in the local communities. In terms of language they could be outstanding, and some of the reports still have a literary value. Several of them provide thorough descriptions as regards to social and cultural affairs of the local communities, and their content could go far beyond traditional medicine. One may justly regard many of the reports as excellent topographic renditions in the spirit of Hans Strøm.
Professor Anders Forsdahl in Tromsø has done more than anyone else to bring the old medical reports back to light and put them into a new context. He is worth quoting: «….the vast array of information that is gathered in these report gives…a good picture of the living conditions of the population across our country, and the reports represent a unique source of information in a number of ways.» (20,21).
It has also been well known that the reports contain landmarks in medical history, that is discoveries or observations that have been unique nationally, and even internationally. Two such examples – which Forsdahl also describes – is the later district physician Andreas Christian Bull (1840–1920) who in his medical report from the municipality of Søndre Odalen in 1868 as the first ever in Norway, and probably the world, described a polio epidemic (21). The other is district physician Johan Christian Lund’s (1830–1906) first time description of Chorea Huntington-Lund in the medical report from Setesdalen in 1860 (fig 5). There are also lesser landmarks. In the medical report from Fredrikshald in 1804 from town surgeon Johan Wittkugel (1755–1829) he told that in May 1804 he was summoned to two small girls who «had left their minds and become as insane».
«They were intensely attacked by convulsions, confusion of their senses, gritting of teeth etc.» In the children’s pockets there was found «entire pieces of henbane roots», hence it was a case of henbane poisoning (Hyoscyamus niger). The situation, the symptoms and the treatment are properly described, and this is probably the first time this condition has been described in medical terms in this country (12).
The doctors often seized the opportunity in the medical reports to comment on the appearances and causes of diseases. As early as in 1804 county physician Christian Jesper Seip (1751–1806) in the county of Smaalenene commented on the causes of «radesyke» (12) Around 1800 it was a not unusual opinion that such patients might be subject to diet, and in particular the consumption of fish was mentioned. With a keen ability to observe as well as common sense, Seip boldly countered such a notion: «…I already doubt, that the eating of fish plays so much of a part, as is generally assumed, as at the Hvaløerne (a group of islands just off the coast), which is where in the district that most fish is being caught and eaten, I have so far never during my time in this office encountered one who has been ill of this kind, whereas there are even several from other parishes, where the general public rarely or never enjoys fish…»
The 19th century is known as a dynamic century, with major ideological and philosophical controversies. This is reflected in the medical reports as well, i.a. in the view on «the veneral disease». In his medical report for Hedemarken county of 1820, county physician Christian Lintrup (1768–1844) expressed grave concern over the increase in «the number of veneral patients» and commented that he found the cause of «the ever increasing occurrence of veneral diseases, is unobjectionably the among the public too frequent so-called night running…», that is the nocturnal visits to maidens in the country (22). He was aware that this was an age old custom, but because of what he taught was their correlation with the increasing occurrence of sexually transmitted diseases, he campaigned hard against the nocturnal visits in writing as well as in speech. Lintrup had studied in Copenhagen towards the end of the 18th century, and was understandably influenced by the liberalism and optimism of the age of enlightenment. Towards health problems his actions and arguments were predictably rationally based. In his objections to the nocturnal visits, the physician was joined by the clergy. The arguments of the clergy, however, were motivated by the public’s increasing «vice», which was measured by the number of children born out of wedlock.
The opinions of the clergy and the medical profession on the general morale coincided increasingly as the doctors from the era of enlightenment were reduced in numbers. This we can see documented in the extensive reports from district physician Christoffer Munthe (1816–84) in southern Østerdalen district. In his voluminous and interesting report fra 1871, he wrote about the proliferation of vice, laxity and lewdness among substantial parts of the population, and reminisced about those days where «there still was domestic as well as infant discipline», and the «sermon and hymn books still did not have to share space over the high seats with neo-political newspapers and rationalist writings»(23) (fig 6). The ideas in vogue were now the conventional and moralist Victorianism with its utilitarian philosophy, materialism and transfer of responsibilities unto the individual. As most people, Munthe and his colleagues were products of their times.
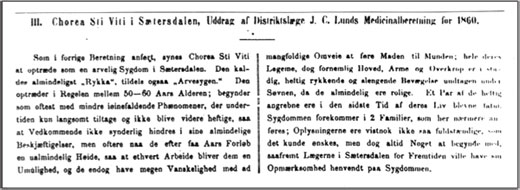
Fig 5. Cut from the first description of Chorea Huntington-Lund in the National medical report of 1860.
There are several such examples in the medical reports. In 1896, district physician Johan William Welle (1851–1915) in Rendalen wrote that «their (the workers’) poverty is mainly due to a lack of sense of any kind of economy and the incompetence of the women regarding all kinds of domestic activities…» (24).
It is difficult to document that the 19th century doctors had particularly liberal political or social views. They were as most public servants, serious about the execution of their duties, somewhat pompous and usually certain about their own authority. The medical reports hardly suggest that they were characterized by a particularly humanistic mind, which one perhaps would have thought from the ideology that many of them considered the basis of their chosen profession. It was rather a distinct sense of duty that was the backdrop of their selfless endeavours, and this encompassed a traditional paternalistic attitude towards their patients.
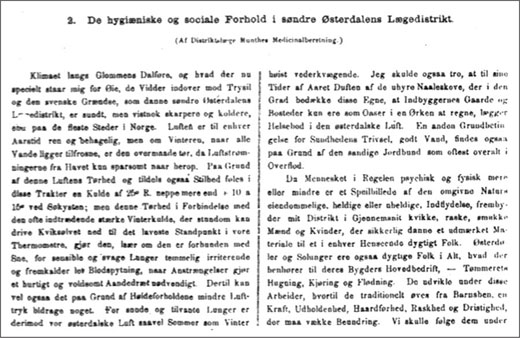
Fig 6. Medical report from the district of Søndre Østerdalen by district physician C. Munthe. Printed as an appendix to the National report of 1871.
The significance of the reports
Particularly during the 19th century, the edited reports constituted an important fundament for decisions on health policies, because the Ministry to a large extent relied on these when giving policy advice. During this period, the reports documented the most important preventive measures available to society concerning important public health problems such as acutely contagious diseases and infant mortality. This applies particularly to tracking and isolation, the vaccination against smallpox and the expansion of midwife services in the districts. These measures and their significance have been described more extensively by Ole Georg Moseng (5). The emphasis the health authorities put upon these preventive measures also appears from the national report of 1814 (13). Here all doctors were listed who had submitted «the ordered medicinal report», as well as all those who had neglected to do so! (fig 7). In the report, the handful of doctors who had made great efforts regarding the vaccination and other public duties pertaining to their offices were also hailed and mentioned by name.
With the modernization of the country more sources of information arose, and new information technology and knowledge contributed hereto. As a consequence, the importance of the medicinal reports as a source of information decreased. The increased role of the media as a provider of input to the political process during the 20th century should not be underestimated in this regard.
A reading of the reports after World War I shows that they almost dried up. They presented a more anonymous expression than previously, and no longer had the broadly informative value as they used to have. As of the 1960s it became clear that their rigid form no longer was adapted to the new panorama of diseases and the change in risk factors towards the public health. In that form the reports hade become obsolete when they ceased to be written in 1984. In the 18th century however, public doctors and their reports were significant to the local level primarily in that they established the political importance of public health, they inspired debates within the expanding and ever more politically conscious urban middle class and among the farmers in the countryside. At the same time, the doctors were able, through the health commissions and the reports, to identify local hygienic problems with a bearing on public health. This is well documented, i.a. through studies initiated by the District College of Bø, Telemark (25).
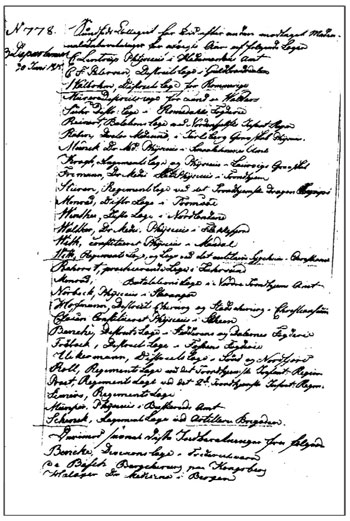
Fig 7. Cut from the central report to the ministry in 1815. The names of the doctors who had presented their reports are listed, as well as those who had not. National archives.
The medical reports today
In addition to various purposes of education, i.a. at the higher institutions of health education and the departments of medicine, the reports are used to today primarily as a source for studies of cultural and social history. The most prominent example is the two volume work on the history of the health services in connection with their 400 years anniversary in 2003 (26). The town and country books, and other local history related literature of the history of local communities, have during the last decades increasingly been professionalized. Now, many of these authors – often historians – actively employ the medical reports of the national archives as a main source of reference in writing social and health history of the community or municipality (Ola Alsvik, historian, personal account.).
This literature has successively been ever improved in presentation and, not least, content. They attract a wide readership, and there is allegedly a moderate, but increasing number of articles on subjects of cultural history based on, among other sources, the medicinal reports. In particular did the 400 years anniversary of the health services in 2003 inspire this development. This indicates that the medical reports will be of increased prominence locally in the future, and it is not hard to agree with the following statement: «The local reports, as a rule recorded in the old gothic handwriting, are best suited for local studies, and they are often used for this purpose»(27).
The regional and central medical reports have been subject to better quality testing than the local reports, and best suited for research. The most important example, and where the medical reports have contributed significantly to the underlying source material is «The Shaping of a Profession, Physicians in Norway, past and present». This is the result of a project cutting through academic boundaries, which analyzes the rise of Norwegian doctors and the health services from a number of academic vantage points (28).
The number of future users of these sources seems to be increasing, as demonstrated by the newly established «National inter-academic network for medical history» rooted in circles of social science at the universities in Bergen and Trondheim. Just like other archives of sources in cultural history it is therefore desirable that they be more accessible, through means such as transcriptions and the Internet.
References:
Canc.Circul (til samtlige Øvrigheder i begge Riger), ang. hvad af Lægerne til Øvrigheden, og af denne til Sundheds-Collegium aarligen skal indberette. Wessel Berg FA. Kongelige Rescripter, Resolutioner og Collegial-Breve for Norge 1660–1813. Bd 4, 1797–1813. Christiania: Cappelen 1845.
Schou JR. Chronologisk Register over de Kongelige Forordninger og aabne Breve som fra Aar 1670 ere udkomne, tilligemed et nøiagtigt Udtogt af de endnu gjeldende forsaavidt samme i Almindelighed angaae Undersaaterne i Danmark og Norge. VIII Deel 3die Stykke. Kiøbenhavn, 1784.
Blomstedt Y, Frohnert P, Gustafson H, Jørgensen H, S, Nagel A-H, Peterson C, Suphellen S, Vuorensola H. Administrasjon i Norden på 1700-tallet. Oslo: Universitetsforlaget, 1985.
Frd. om Medicis og Apothekere. 4 December 1672. Tangberg KA, Esmark-Olssøn L, Sømme, J. Norsk Medicinallovgivning 1672–1880. Kristiania: Justisdepartementet, 1881.
Moseng OG. Det offentlige helsevesen i Norge 1603–2003. Bd.1. Ansvaret for undersåttenes helse 1603–1850. Oslo: Universitetsforlaget, 2003.
Malm O. Kopper og vaccination i Norge. Kristiania: Aschehoug, 1915.
Frd. for Danmark og Norge, ang. Vakcinationen. Fangberg KA, Esmark-Olssøn L, Sømme J. Norsk Medicinallovgivning. Kristiania: Justisdepartementet, 1881.
Bjorvatn B, Danielsen A. Radesyken – en norsk tragedie. Tidsskr Nor Lægeforen 2003;123: 3557–8.
Lie, AK. Tanker om radesyken i Norge – «Den hentærer sine Ofre langsomt». Tidsskr Nor Lægeforen 2003;123:3562–4
Stolt C-M. Den beprovade erfarenheten. Medicinsk idéhistorie och läkarekonst i Boråsbygden 1780–1900. Borås: Norma Förlag, 1994.
Canc.prom. (til verdslige Overøvrigheder og nogle, maaskee alle Biskopper) 24. Januar 1807. Tangberg KA, Esmark-Olssøn L, Sømme J. Norsk Medicinallovgivning 1672–1880. Kristiania: Justisdepartementet 1881.
Medisinalmeldingene 1804. Rapport fra Helsetilsynet 6/2004. Oslo: Statens Helsetilsyn, 2004.
Riksarkivet. Sundhedskollegiet 1809–1815. Pk. 15–18. Hyllenr. 4A00443.
Larsen Ø (red.) Norges leger 1996. I-V. Oslo: Den norske lægeforening, 1996.
Dyrvik S. Den lange fredstiden 1720–1784. Bd. 8 i Mykland K (red.) Norges historie. Oslo: Cappelen, 1978.
Falkum E. Sykdomsoppfatning, helseomsorg og samfunn. Oslo: Universitetsforlaget, 1978.
Bestemmelser for Afgivelsen af de Medicinalberetninger, som Rigets samtlige Læger i Følge Kgl.Res. af 13 Februar 1807 have aarligen at indsende til Medicinalstyrelsen. Kgl. Resolution 17 December 1864. Tangberg KA, Esmark-Olssøn L, Sømme J. Norsk Medicinallovgivning 1662–1880. Kristiania: Justisdepartementet, 1881.
Brock G. Bemærkninger til Levemaaden og de hygieniske Forhold i indre Hardanger Distrikt. Anhang til Medicinalberetningen for søndre Bergenhuus Amt. I: Beretning om Sundhedstilstanden og Medicinalforholdene i Norge i 1855. Christiania: Departementet for det Indre, 1857.
Holmsen H. Bemærkninger om de hygieniske Forhold i Midthordlands Distrikt og Beretning om de der oprettede Sundhedscommissioner. Anhang til Medicinalberetningen for Søndre Bergenhuus Amt. I: Beretning om Sundhedstilstanden og Medicinalforholdene i Norge i 1855. Christiania: Departementet for det Indre, 1857.
Forsdahl A. Sunnhetstilstanden, hygieniske og sosiale forhold i Sør-Varanger Kommune 1869–1975 belyst ved medisinalmeldingene. ISM skriftserie no.2. Tromsø: Institutt for samfunnsmedisin, Universitetet i Tromsø, 1992.
Forsdahl A. Merkesteiner i norsk medisin reist av almenpraktikere og enkelte udrag av medisinalberetninger av kulturhistorisk verdi. ISM skriftserie no. 8. Tromsø: Institutt for samfunnsmedisin, Universitetet i Tromsø, 1984.
Medisinalberetning 1820 for Hedemarkens amt. Katalog 1252/01. Riksarkivet.
Munthe C. De hygieniske og sociale Forhold i søndre Østerdalens Lægedistrikt. I: Beretning om Sundhedstilstanden og Medicinalforholdene i Norge 1871. Medisinalberetning for Hedemarkens amt. Christiania: Departementet for det Indre, 1873–4.
Wille JW. Medisinalberetning for Rendalen legedistrikt 1896. Katalog 1263/50. Riksarkivet.
Storesund A. Sunnhetskommisjonens virke i 5 herreder i Telemark 1861–1900. Tidsskr Nor Lægeforen 1999;119:4547–52.
Schiøtz A, red. Det offentlige helsevesens historie 1603–2003 I-II. Oslo: Universitetsforlaget, 2003.
Larsen Ø. Diseases, geography and attitudes. I: Larsen Ø, ed. The shaping of a profession. Canton MA: Science history Publications/USA, 1996.
Larsen Ø, ed. The shaping of a profession. Canton MA: Science history Publications/USA, 1996.
County medical officer (ret.)
Kongsveien 37 B
N–2380 Brummunddal
