Eli Feiring, Carl Tollef Solberg
Priority setting of COVID-19 vaccines in Norway: Advice and process
Michael 2021; 18: Supplement 28: 49–60 (Norwegian version 49–59)
In the autumn of 2020, the Norwegian Institute of Public Health invited us to participate in an external group that would be advising on COVID-19 vaccine priority-setting in Norway. The group’s mandate was to set goals for the Norwegian National Coronavirus Immunisation Programme, as well as to provide general recommendations regarding priority groups in the first phase of the vaccine deployment. The group recommended prioritising the risk group and healthcare personnel and also proposed geographical prioritisation depending on community case incidence. The group’s advisory report was part of a large-scale multidisciplinary project comprising epidemiology, medicine, infection control, computer modelling of COVID-19 vaccine efficacy and economic cost-benefit analyses. Priority setting implies that some citizens are given preference ahead of others who must wait. In Norway, as elsewhere, there is disagreement concerning the values, principles and goals determining vaccine prioritisation. In this article, we present an account of the group’s work process, advice, and rationales in more detail and identify values-based ‘trade-offs’ that pose particular challenges.
«(D)ecisions about how to deploy limited COVID-19 vaccines should not be based on only public health considerations. Nor should they be driven by economic considerations alone» (WHO 2020:5).
Introduction
Within the first months of 2020, the novel coronavirus, SARS-CoV-2, caused a global pandemic. To date (as of 1 March 2021), worldwide, the cumulative number of confirmed cases is 113.8 million and the number of confirmed fatalities is 2.5 million (1). Extensive infection control measures have been implemented in most countries at immense societal cost.
On 12 March 2020, Norway went into national lockdown. In the absence of any vaccine and with limited options for treating COVID-19, a number of restrictive measures were introduced to limit transmission. These infection control measures impacted the population’s personal freedoms, employment, and economic activity (2).
In the summer of 2020, the race to develop COVID-19 vaccines gathered pace, and by late autumn, almost 50 vaccine candidates were undergoing large-scale clinical trialling (3). The hope was that the efficacy of the coming vaccines would be sufficient to stem the pandemic and ease the burden of severe disease for the individual, for the health service, and for society – and the burden of the comprehensive infection control measures. Norway was an early party to the EU Advance Purchase Agreement on vaccines procurement. The expectation was that demand for vaccines would exceed supply and thus necessitate prioritisation of who could come first in line for the vaccination.
In the autumn of 2020, we were invited to participate in an external expert group that would provide ethics-based advice on vaccine priority setting. This expert group – referred to hereafter as the ethics advisory group – was appointed by the Norwegian Institute of Public Health as one of many elements in developing the Norwegian Coronavirus Immunisation Programme. The mandate was to set goals for the Programme, and to provide general recommendations regarding priority groups in the first phase of vaccination. The report of the ethics advisory group was submitted on 15 November 2020 (3).* Eli Feiring was one of the six appointees to the ethics advisory group, and Carl Tollef Solberg worked in the secretariat. Both Feiring and Solberg are listed as co-authors of the report. The following individuals were appointed: Eli Feiring (University of Oslo), Reidun Førde (University of Oslo), Søren Holm (University of Oslo/University of Manchester), Ole Frithjof Norheim (University of Bergen), Berge Solberg (Norwegian University of Science and Technology) and Gry Wester (King’s College London). The secretariat consisted of Jasper R. Littmann (Head of Secretariat, Norwegian Institute of Public Health), Trygve Ottersen (Norwegian Institute of Public Health) and Carl Tollef Solberg (University of Oslo/Norwegian Institute of Public Health). The opinions expressed in this publication are those of the two authors of the article alone.
The public debate that ensued has revealed how differing considerations stand relative to each other and that clarification of their underlying principles is required. In the following, we will be detailing the ethics advisory group’s advice and work process: Part 2 describes the work process. In Part 3, we present the ethics advisory group’s interim recommendations. Part 4 discusses the normative framework and some of the empirical premises on which the ethics advisory group’s advice relies, and in Part 5, we briefly examine specific ethical challenges. In Part 6, we round off the article with concluding comments.
Process
The Ministry of Health and Care Services commissioned the Norwegian Institute of Public Health to establish a Norwegian National Coronavirus Immunisation Programme. The Programme was organised into five main areas: implementation, recommendation and prioritisation, monitoring, communication, and research (4). The ethics advisory group was one of several groups within the area of recommendation and prioritisation. The Norwegian Institute of Public Health was responsible for adapting and implementing the Norwegian National Coronavirus Immunisation Programme and for the final priority order.
The ethics advisory group consisted of academics with extensive expertise and experience in the field of priority setting and with a specialist background in medicine, philosophy, and political science. The Norwegian Institute of Public Health’s secretariat assisted by ensuring coordination with the Norwegian National Coronavirus Immunisation Programme.
The ethics advisory group’s mandate did not extend to take account of the specific interests of the health service, clinicians, the risk group or critical societal functions. Instead, the ethics advisory group was tasked with providing general advice informed by the values framework for health priority-setting in Norway, taking into account international interim recommendations, including those of WHO.
The ethics advisory group’s work was carried out from late September until early November, and the group convened for six meetings.
Interim recommendations
The ethics advisory group recommended a dynamic priority setting model (Figure 1). In a scenario where transmission is under full or partial control, the ethics advisory group advised giving first priority to the risk group and to healthcare personnel. In a scenario of escalating transmission, the ethics advisory group recommended that healthcare personnel be given priority over the risk group and that critical societal functions might be considered as a third priority group. The intention was not for these general priorities to be lexical, i.e., that the entire risk group should take priority over the healthcare personnel group or vice versa. Rather, the idea was that the highest-ranking main priority group should be given a somewhat greater weighting than the next priority group. Furthermore, the recommendation was that priority should be given to geographical areas with a high reproduction rate in a high case-incidence scenario.
The advice on prioritising the risk group and healthcare personnel, and giving consideration to dynamic prioritisation, was largely adopted by the Norwegian health authorities (4).*Norwegian Institute of Public Health. Who will get the coronavirus vaccine? https://www.fhi.no/en/id/vaccines/coronavirus-immunisation-programme/who-will-get-coronavirus-vaccine-first/ (Last accessed 31/01/21). In January 2021, agreements were made with several vaccine manufacturers and immunisation of the Norwegian population commenced.
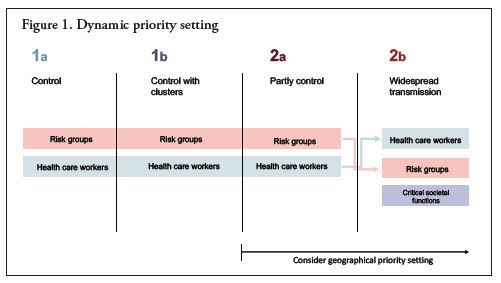
Figure 1. This figure illustrates the ethics advisory group’s proposed dynamic priority setting. As the figure shows, the premise was that increased transmission in society would support the rationale of prioritising healthcare personnel. In the event of a high transmission rate, the ethics advisory group consequently proposed giving healthcare personnel priority over the risk group (3).
Rationale
Within any nation (and not least amongst different nations), disagreements concerning values and the relative weighting of different considerations are inevitable. Uncertainty concerning ethics often stems from empirical uncertainty: the scientific evidence for a given concern may constitute a substantive difference in ethics. In ethical analysis, where the aim is to arrive at a reasoned decision, it may thus be necessary to procure information about the consequences of the various alternatives: who would be affected, and in what way? This entails possessing the specialist insight for evaluating such information and determining its applicability and weighing it up against various ethical considerations.
Recommendations under empirical uncertainty
The work of the ethics advisory group was based on the evidence available in the autumn of 2020. With the assistance of the other groups under the Norwegian Institute of Public Health, the ethics advisory group had access to up-to-date information on the COVID-19 vaccines, the risk group, infection risk within occupational groups, and logistical challenges involving the vaccine candidates that were on the way. Meanwhile, however, information concerning a number of other factors was scarce at that stage of the pandemic. There was, for instance, uncertainty concerning the efficacy of the vaccines, their potential adverse effects, which groups the different vaccine candidates would have been trialled in and approved for, public uptake of the vaccines and, not least, what course the pandemic would take.
The expected efficacy of the vaccines became a key factor. The vaccine candidates in question proved effective in reducing morbidity and mortality, while their effectiveness for infection control remained unclear (4). The evidence as it existed in November 2020 indicated that the vaccine would have the most benefit as a means of preventing severe illness and fatalities as opposed to preventing community transmission.
Values, goals, and priority groups
To develop an ‘ethics framework’, in the sense of a set of principles and values to inform policymaking, the ethics advisory group largely based the defining values on those otherwise applied in Norwegian healthcare. This is discussed in several Norwegian official reports (5–6). Further, Norway has a long-standing tradition of transparency in its priority setting in health care, and both the national legislation and official guidelines are drawn up in consultation with priority setting committees (7–11). Three formal criteria are applied in guiding priorities in the Norwegian public health service: The health-benefit criterion, the resource criterion, and the severity criterion.
Preventive public health measures cannot generally be compared with prioritising individualised and (potentially) curative healthcare. For this reason, a recent Norwegian priority setting white paper recommended that priority setting of public health measures be addressed as a matter in its own right (6,12). Indirect health benefits are important: a vaccine benefits others in addition to the vaccinee in that it reduces community transmission. In the programming documents for severe communicable diseases, such as pandemic influenza, for example, several prioritisation factors are identified: The main premise is that the risk group, practising healthcare personnel and defined key individuals should be given priority over the general population (13).
The ethics advisory group also consulted international literature on priority setting of vaccines. A number of publications have documented different countries’ priority setting recommendations (3). In particular, the WHO SAGE values framework for prioritization of COVID-19 vaccination is intended as decision support for national strategies (14).
The ethics advisory group advocated that the Norwegian National Coronavirus Immunisation Programme should be predicated on the following values: equal respect, welfare, equity, trust, and legitimacy. In the Norwegian context, the principle of equal respect is a norm of particular relevance, being linked both to official standards of non-discrimination and needs-based equitable access to healthcare, and to the goal of reducing social inequalities in health. Further, the health-benefit value is focal: Scarce health resources should be distributed to maximise their benefit and increase overall national (health-related) welfare. At the same time, procedural considerations are important. The Norwegian National Coronavirus Immunisation Programme should be founded on trust between the public and the authorities, and the allocation of vaccines should be defensible and justifiable with respect for the entire population, including those who do not receive the vaccine (15).
Based on this, the ethics advisory group proposed the following goals for the Norwegian National Coronavirus Immunisation Programme: reduce the risk of severe illness and death, maintain essential services and critical infrastructure, protect employment and the economy, and reopen society.
Specific ethical challenges
In many respects, the public debate that ensued from the ethics advisory group’s report reflected a number of the discussions within the group. One example of this is the discussion concerning the objective of the Norwegian National Coronavirus Immunisation Programme: In general terms, immunisation will be one of several pandemic countermeasures, and the benefit of the Norwegian National Coronavirus Immunisation Programme will thus depend on what other infection control measures are deployed. We have no way of knowing how the Programme’s different goals should be ranked if all such goals are not achievable concurrently. Rather than prioritising relative risk reduction for serious illness and death, it may be argued that immunisation should operate with a broader goal: of protecting against any harmful effects of the pandemic and infection control measures, and the consequences for life and health must be weighed up against other societal consequences such as limitation of civil liberties and financial loss.*Steinar Holden’s posting translating as “it is not a given that health and severe illness definitively take priority in vaccination” in DN 19/11/20/29/11/20 https://www.dn.no/okonomi/koronaviruset/koronadebatt/vaksine/kronikk-det-er-ikke-gitt-at-helse-og-alvorlig-sykdom-skal-ha-absolutt-prioritet-ved-vaksinering/2-1-914022 (Last accessed 28/01/21), as well as a rejoinder posted by S. Holden translating as “the aim of the immunisation strategy is to reduce all the adverse effects of the pandemic” in DN https://www.dn.no/innlegg/koronaviruset/koronadebatt/helse/innlegg-malet-med-vaksinasjonsstrategien-er-a-redusere-alle-pandemiens-skadevirkninger/2-1-920556 (Last accessed 28/01/21). Another example is the discussion concerning the priority setting of socioeconomically disadvantaged groups. The burden of disease is unequally distributed. In a number of countries, social inequalities in health have been exacerbated by the pandemic (16). The national infection control measures have heavily affected socioeconomically disadvantaged groups. The ethics advisory group emphasised that early vaccination of the risk group might permit faster reopening of society and thereby benefit socioeconomically disadvantaged groups. Owing to space constraints, we are unable to discuss this topic further, and concentrate instead on three other ethical challenges.
Vaccinate to gain life years or save lives?
The most common approach in healthcare priority-setting is to quantify the benefit of an intervention in terms of quality-adjusted life years (QALYs). For priority setting of COVID-19 vaccines, however, QALYs are not a viable option due to the scarcity of evidence-based data.
The ethics advisory group discussed whether the vaccine should be aimed at gaining life-years or preventing fatalities. All things being equal, many people will assert that it is more important to prevent deaths among young individuals than among elderly persons. This then suggests life years as a reasonable measure. However, the infection fatality ratio, indicating the risk of dying if infected, is extremely low among the young healthy individuals in Norway but high among the oldest. The large age-dependent difference in the infection fatality ratio implies that it is reasonable to assume that prioritising life or life years will not constitute a significant difference when weighing up benefit* See also Ole Frithjof Norheim’s example calculation. This calculation shows that the choice between life or life years has no material significance in the main priority setting strategy for the risk group versus healthcare personnel: “Slik valgte vi hvem som får vaksinen først”[How we decided who should get the vaccine first] Morgenbladet 04/01/21. https://morgenbladet.no/aktuelt-ideer/2020/12/slik-valgte-vi-hvem-som-far-vaksinen-forst (Last accessed 01/03/21). : older individuals should be given priority over younger individuals both if life years are to be gained and if fatalities are to be prevented by immunising large groups in society.
The ethics advisory group was divided on the question of whether to use life years or life as a measure but ultimately settled on life – with the key assumption that life years and life would result in a fairly equal prioritisation of groups. Life is a transparent measure in the sense that it is easily understood. Life is also helpful for data modelling. Life years, on the other hand, can be modelled as a measure in several ways, and it could be argued that the life-years goal embodies a number of theoretical value assumptions (such as the quantitative norm for lost QALYs defined for each age group). At the same time, the ethics advisory group proposed that a switch might be made to life years gained if it subsequently emerged that this measure yielded significantly greater health-benefit value from the Norwegian National Coronavirus Immunisation Programme.
These assessments were made in light of the evidence available at that time. The ethics advisory group had no evidence-based data on vaccine efficacy for reducing viral transmission and concluded that case fatalities could best be reduced by vaccinating the risk group first.
Should healthcare personnel be given first priority?
Some have advocated giving healthcare personnel first priority for the COVID-19 vaccine, regardless of risk profile, the overall infection situation and the infection control efficacy of the COVID-19 vaccines. In principle, this could be implemented in several ways. For example, all or a selected proportion of the healthcare personnel group could take lexical priority, i.e., come before the first individual in the risk group. Alternatively, healthcare personnel and the risk group could be prioritised concurrently in (at least) two ways: either by ensuring that healthcare personnel are guaranteed a larger share of the vaccine doses or by healthcare personnel (smaller group) having a greater likelihood of being vaccinated than people in the risk group (larger group).
There are many reasons for prioritising healthcare personnel. One argument is reciprocity: society has called on certain occupational groups – such as frontline healthcare personnel – to expose themselves and hence their immediate relatives to infection risk.* A reciprocity argument may in principle apply to any group in society exposed to a significant risk of infection, including shop assistants, hospital laundry workers or taxi drivers. Preliminary figures for Norway (for the year 2020) show that cleaners (1.66%) and paramedics (1.71%) were the groups with the highest incidence, excluding those infected abroad. As expected, nurses (1.55%) and doctors (1.39%) had a somewhat higher incidence (excluding those infected abroad) than the Norwegian general population of working age (1.11%). However, health workers such as clinical psychologists (0.69%) and physiotherapists (0.89%) had a lower incidence than the general population (16). The reciprocity argument dictates that those who run an extra risk are entitled to extra protection. Those who ‘give’ something extra deserve something extra in return. None of the three Norwegian priority criteria – health-benefit, resource, or severity – justify, even in principle, that the reciprocity argument should carry any weight. Meanwhile, it could be argued that frontline healthcare personnel in frequent contact with patients should be protected against communicable disease on the grounds of health-benefit alone – to at-risk patients, to themselves and to their immediate relatives. Moreover, there is justification for prioritising those who would otherwise be difficult to replace if they succumb to illness or have to quarantine: as ‘insurance’ to prevent the collapse of the health service during the pandemic. These last-named factors are covered by the principles of the health-benefit criterion and were emphasised by the ethics advisory group.
Should geographical priority setting be rejected?
The equal respect principle has a strong standing in the Norwegian health service and also includes a commitment to geographical equal respect. The Patient and User Rights Act is intended to ensure equal access to high-quality services. Nevertheless, the ethics advisory group judged that geographical factors could be weighted in order to prioritise parts of Norway with a particularly high and persistent transmission rate, in order to reduce both the risk of disease in the individual and the risk of overloading the health service and in order to reduce the need for other infection control measures. Meanwhile, the group responsible for the socioeconomic cost-effectiveness of COVID-19 immunisation concluded: “If we do not prioritise the population in parts of the country that are most heavily affected, costly infection control measures will need to remain in place for longer than strictly necessary, with implications for the whole country’s economy” (18: 5).
The ethics advisory group advocated that geographical prioritisation should be considered under certain conditions. * One issue that was scarcely addressed concerned who should actually benefit from geographical priority setting. Such priority setting would presumably target the risk group (i.e., reduce morbidity and mortality), healthcare personnel (i.e., guarantee capacity) and epidemiological interventions to control infection. On 2 March 2021, the Norwegian Institute of Public Health recommended a slight geographical bias.* For some time, the Norwegian Institute of Public Health judged that the conditions for geographical targeting were not met: on the one hand, because the course of the pandemic is unpredictable and the effects of the vaccine are not achieved until several weeks after it is administered, and on the other hand because the Institute’s advanced data modelling indicated that vaccine benefit is greatest in geographical regions with either a particularly low or particularly high transmission rate (4). The last-named finding no doubt seems counterintuitive if the assumption is that the vaccine has the most benefit in regions where the transmission rate is highest. Increasing use of and confidence in the findings of advanced data modelling makes the priority setting debate less transparent.
The assessment of geographical prioritisation exemplifies how empirical uncertainty impacts the trade-off between benefit and equal respect: if the benefit of geographical prioritisation is unequivocal, geographically equal access to the vaccine will have to cede.
Conclusion
Priority setting stirs public engagement, especially when it concerns COVID-19 vaccines. COVID-19 vaccines are a scarce resource that much of the Norwegian (not to mention the global) population is keen to gain access to, stands to benefit from and, not least, is legitimately entitled to. Furthermore, priority setting concerning this particular vaccine involve not only public health and the health service but the nation as a whole.
The work of the ethics advisory group was one element in a major development project involving a number of employees of the Norwegian Institute of Public Health. In sum, this large-scale project provided the basis for the detailed priorities the Institute recommended to the Norwegian Government. The recommendations of the ethics advisory group as of November 2020 for placing the risk group and healthcare personnel first in line were interim recommendations and have continuously been subject to change. Priority setting of COVID-19 vaccines is and should be dynamic, and the Norwegian Institute of Public Health has duly held regular meetings with the Norwegian Medical Association, the Norwegian Nurses Organisation, the Norwegian Dental Association and the Norwegian Association of Local and Regional Authorities (KS).
A large proportion of the Norwegian public and a number of politicians appear to have acknowledged the necessity of prioritising COVID-19 vaccines. We, therefore, round off this article with two hopes. The first is that public debate about the priority setting of vaccines will advance the priority setting discourse in Norway. The second is that discussions concerning vaccine prioritisation, infection control measures and reduced hospital capacity have served to give the general public a better understanding of the need to set explicit priorities. Such priority setting should be conducted transparently and based on evidence and fundamental principles. We are optimistic.
References
WHO. 2021. WHO Coronavirus disease (COVID-19) Dashboard. https://covid19.who.int (Last accessed 31/01/21).
Holden S, Bjørnland H, von Brasch T, et al. (2020) Covid-19 – samfunnsøkonomisk vurdering av smitteverntiltak – andre rapport. Rapport fra ekspertgruppe på oppdrag for Helsedirektoratet. [Socioeconomic evaluation of infection control measures – second report of the expert advisory group commissioned by the Norwegian Directorate of Health.] 22 May 2020. https://www.helsedirektoratet.no/rapporter/samfunnsokonomisk-vurdering-av-smitteverntiltak-covid-19 (Last accessed 31/01/21).
Feiring E, Førde R., Holm S, et al. (2020). Advice on priority groups for coronavirus vaccination in Norway: Expert group in ethics and priority setting, 15 November 2021. Norwegian Institute of Public Health. https://www.fhi.no/contentassets/9d23593d6ebe443ba12556d3f7284eb8/norwegian-ethics-advisory-report-for-corona-vaccination.pdf (Last accessed 26/01/21).
Norwegian Institute of Public Health (2020). Koronavaksinasjonsprogrammet: Folkehelseinstituttets foreløpige anbefalinger om vaksinasjon mot covid-19 og om prioritering av covid-19-vaksiner, versjon 2. 15. desember 2020. [The Norwegian National Coronavirus Immunisation Programme: The Norwegian Institute of Public Health’s interim recommendations for vaccination against COVID-19 and on prioritisation of COVID-19 vaccines, version 2. 15 December 2020.] Norwegian Institute of Public Health. https://www.fhi.no/contentassets/d07db6f2c8f74fa586e2d2a4ab24dfdf/2020-12-v2-anbefalinger-og-prioriteringer-2-utgave-korrigert-forside.pdf (Last accessed 31/01/21).
Norwegian Institute of Public Health (2014) Social inequalities in health. I: Public Health Report – the current state of health in Norway. Oslo: Norwegian Institute of Public Health. https://www.fhi.no/en/op/hin/groups/social-inequalities/
Meld. St. 34 (2015–2016). Principles for prioritisation in healthcare — Summary of a white paper on prioritisation in the Norwegian healthcare sector. Oslo: Ministry of Health and Care Services. https://www.regjeringen.no/en/dokumenter/meld.-st.-34-20152016/id2502758/?ch=1 (Last accessed 26/01/21).
NOU 1987:23. Retningslinjer for prioritering innen norsk helsetjeneste. [Guidelines on priority-setting in Norwegian healthcare.] Official Norwegian Reports. Oslo: Ministry of Health and Care Services.
Lønning I, et al. (1997). Prioritering på ny – Gjennomgang av retningslinjer for prioriteringer innen norsk helsetjeneste. [Re-prioritisation: Review of guidelines for prioritisation in the Norwegian health service.] NOU 1997:18. Official Norwegian Reports. Oslo, Norway: Ministry of Health and Social Affairs. https://www.regjeringen.no/no/dokumenter/nou-1997-18/id140956/ (Last accessed 31/01/21).
NOU 2014:12 Åpent og rettferdig – prioritering i helsetjenesten. [Official Norwegian Report 2014:12 Transparent and fair – priority-setting in Norwegian healthcare] Official Norwegian Reports. Oslo: Ministry of Health and Care Services. https://www.regjeringen.no/no/dokumenter/NOU-2014-12/id2076730/ (Last accessed 31/01/21).
NOU 2018:16 Det viktigste først – Prinsipper for prioritering i den kommunale helse- og omsorgstjenesten og for offentlig finansiert tannhelsetjenester. [Official Norwegian Report 2018:16 The most important thing first – Principles for prioritisation in the municipal health and care service and for publicly funded dental health services]. Official Norwegian Reports. Oslo: Ministry of Health and Care Services. https://www.regjeringen.no/no/dokumenter/nou-2018-16/id2622153/ (Last accessed 31/01/21).
Haldar M, Ødemark J, Engebretsen E (2020). Helseprioriteringer i endring – en retorisk analyse. [Health care priority setting in change – a rhetorical analysis] Nytt Norsk Tidsskrift 3, 37: 225–237.
Norheim OF (2018). Verdigrunnlag og prioriteringskriterier for folkehelsearbeidet. [Values and prioritisation criteria in public health work. A report commissioned by the Norwegian Ministry of Health and Care Services] https://www.uib.no/sites/w3.uib.no/files/attachments/norheim_notat_om_verdigrunnlag_og_kriterier_for_prioritering_innen_folkehelsearbeidet_181112_0.pdf (Last accessed 31/01/21).
Norwegian Institute of Public Health (2018). Influensa – veileder for helsepersonell [Influenza – guidelines for healthcare professionals] https://www.fhi.no/nettpub/smittevernveilederen/sykdommer-a-a/influensa/ (Last accessed 31/01/21).
WHO (2020). WHO SAGE values framework for the allocation and prioritization of COVID-19 vaccination, 14 September 2020. World Health Organization. https://apps.who.int/iris/handle/10665/334299 (Last accessed 31/01/21).
Daniels N (2008). Just health: meeting health needs fairly. Cambridge: Cambridge University Press.
Kawachi I (2020). COVID-19 and the “rediscovery” of health inequities. Int Journal of Epidemiology, 1-4. doi: 10.1093/ije/dyaa159
Molvik M, Danielsen A S, Grøsland M, et al (2021). SARS-CoV-2 in health and care staff in Norway, 2020. The Journal of the Norwegian Medical Association, 3, 23. doi: 10.4045/tidsskr.20.1048
Norwegian Directorate of Health (2020). Samfunnsøkonomisk vurdering av smitteverntiltak (covid-19) [Socio-economic assessment of infection control measures (COVID-19)] [online document]. Oslo: Norwegian Directorate of Health (last expert update 21/12/20, last accessed 27/01/21). Available from https://www.helsedirektoratet.no/rapporter/samfunnsokonomisk-vurdering-av-smitteverntiltak-covid-19
Acknowledgements
We would like to thank Grete Synøve Botten, Siv Cathrine Høymork, Jasper R. Littmann, Ole Frithjof Norheim, Berge Solberg, and Gry Wester for constructive comments on an earlier version of this article.
eli.feiring@medisin.uio.no.
Political scientist, associate professor and head of the Department of Health Management and
Health Economics, University of Oslo.
c.t.solberg@medisin.uio.no
Medical doctor and philosopher, senior researcher at the Centre for Medical Ethics (CME), University of Oslo.
*Corresponding author.
